JUNIPER
PUBLISHERS- JOJ Ophthalmology
Purpose: To report a case of bilateral
allergic blepharoconjunctivitis and periorbital edema following
chemotherapy with combination regimen of rituximab, bendamustine and
bortezomib.
Case report: A 59-year-old man presented with
bilateral periorbital swelling and blurry vision following three cycles
of rituximab, bendamustine and bortezomib combination chemotherapy for
mantle cell lymphoma. At presentation, visual acuity was 20/25 and 20/20
in the right and left eyes, respectively. Slit lamp examination
disclosed a bilateral periorbital myxedema of both upper and lower
eyelids, as well as bulbar and palpebral conjunctivitis. The patient was
prescribed conservative topical medications and monitored with serial
ophthalmic examinations. At 6 weeks follow up, ophthalmic symptoms
improved with the resolution of blepharoconjunctivitis and periorbital
edema.
Conclusion: Bilateral allergic
blepharoconjunctivitis and periorbital edema were reported following
rituximab, bendamustine and bortezomib chemotherapy. Ophthalmic
examination and preventive measures may be warranted particularly in
patients with combination chemotherapy regimen.
Keywords: Blepharoconjunctivitis; Periorbital edema; Rituximab; Bendamustine; Bortezomib; ChemotherapyIntroduction
Ocular toxicities of anti-cancer medications are
often underestimated as compared to the more serious adverse effects in
other organ systems [1-3].
Concurrent to the development of new chemotherapeutic agents and new
combination regimens, there has been an increase in the number of
reported ophthalmic adverse events following chemotherapy. Although
there is a wide spectrum of ocular toxicities induced by cancer therapy [2-4]
little is known about the ophthalmic toxicities of newer
target-specific cellular molecules intended for specific molecular and
biologic pathways. We present a subject with mantle cell lymphoma who
developed bilateral allergic blepharoconjunctivitis and periorbital
edema following chemotherapy with combination regimen of rituximab,
bendamustine and bortezomib.
Case Report
A 59-year-old man with stage IV mantle cell lymphoma
presented to the outpatient Eye Clinic at Stroger Hospital of Cook
County with the complaint of bilateral periorbital swelling and pain,
burning sensation, and blurry vision for 1 week. The symptoms started 1
week following the third cycle of rituximab, bendamustine and bortezomib
chemotherapy, improved without medications in the time interval between
the third and fourth cycles, and progressed again right after the
fourth chemotherapy cycle at the day of ophthalmic examination. There
was no past ophthalmic history and his past medical history included
peptic ulcer disease. His medications were tylenol, acyclovir,
docusatesenna and pantoprazole. At the initial ophthalmic evaluation,
visual acuity (VA) was 20/25 and 20/20 in the right and left eyes,
respectively. There was a bilateral periorbital swelling and redness
which was not tender on palpation. The patient’s pupils were round and
reactive without an afferent pupillary defect. Extraocular motility was
full and visual fields by confrontation demonstrated no defect.
Intraocular pressure was 12mmHg and 13mmHg in the right and left eye,
respectively.
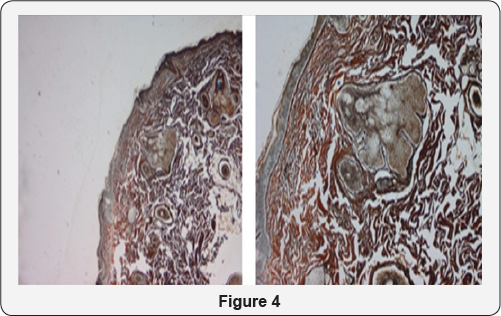
The slit-lamp biomicroscopy disclosed a bilateral
periorbital edema of upper and lower eyelids, and bulbar and palpebral
conjunctivitis. Anterior segment showed corneal irritation and dry eyes
bilaterally, and dilated fundus examination was unremarkable. Review of
systems disclosed right supraclavicular, infra auricular and bilateral
axillary lymphadenopathies, and a rash in the upper chest and upper
extremities. Due to temporal relation between the patient’s ophthalmic
presentation and chemotherapy, his symptoms were attributed to an
allergic reaction to his chemotherapy regimen. Oral diphenhydramine,
topical hydrocortisone lotion, ocular cyclosporine and artificial tears
were prescribed. The patient was instructed to perform warm compresses
and lid scrubs daily, and to return to the clinic two weeks later for
follow up or sooner if urgent symptoms including further vision loss and
eye pain occurred. At 6 weeks follow up, patient showed improvement
with resolution of blepharoconjunctivitis and periorbital edema in both
eyes.
Discussion
Conjunctivitis concurrent with periorbital edema have
been reported following chemotherapy with 5-fluorouracil and
methotrexate [5]. Moreover, isofosfamate [6] Deoxycoformycin [7] doxorbucin [8] Cystosinarabinoside [9] docetaxel, [10] and cyclophosphamide [11] have also been associated with conjunctivitis. Other chemotherapeutic drugs, such as carboplatin, [12]
have been linked to periorbital edema. To our knowledge there have been
no reports of bilateral allergic blepharoconjunctivitis and periorbital
edema following chemotherapy with combination regimen of rituximab,
bendamustine and bortezomib.
Rituximab is a monoclonal antibody against the CD20
antigen of B cells and is used to treat non-Hodgkin B-cell lymphomas.
The most common reported ophthalmic side effects of rituximab include
transient ocular edema, conjunctivitis, burning sensation, and transient
visual changes, [13]
similar to the ophthalmic symptoms of the patient in the current study.
Bendamustine is nitrogen mustard which is used in the treatment of
chronic lymphocytic leukemia and lymphomas [14].
To our knowledge, there have been no reported ocular adverse effects of
bendamustine, but other agents with similar mechanism including
cyclophosphamide may cause blepharoconjunctivitis and reversible blurred
vision [15]. Bortezomib is a proteasome inhibitor and is approved for treating multiple myeloma and mantle cell lymphoma [16]. There have been no reported ocular adverse effects for bortezomib.
The exact underlying mechanism of bilateral
blepharoconjunctivitis and periorbital edema in the patient in the
current study is not clear; however, since the ophthalmic symptoms
started right after each exposure to chemotherapy medications, it is
more likely that the chemotherapy medications caused the symptoms.
Furthermore, both the ophthalmic symptoms and the skin reactions in the
upper chest and upper extremities happened simultaneously, which is
suggestive of allergic reaction to combination chemotherapy. It is not
clear if either rituximab or bendamustine monotherapy or the combination
chemotherapy caused the ocular symptoms in this patient; however, it is
probable that the combination therapy may have increased the risk for
development of ocular toxicities.
Conclusion
In summary, bilateral allergic blepharoconjunctivitis
and periorbital edema were reported following rituximab, bendamustine
and bortezomib chemotherapy. Ophthalmic examination and preventive
measure of allergic reaction may be warranted particularly in patients
with combination chemotherapy regimen.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php