JOJ Ophthalmology- Juniper Publishers
Abstract
Purpose: To evaluate the change in spherical aberration and coma in normal eyes, by employing wavefront-customized hydrogel contact lenses.
Methods: Seven customized, computerized numerically controlled lathe cut hydrogel contact lenses were designed and fabricated incorporating specific amounts of spherical aberration (SA) and coma. Each lens was designed to have only one non-zero Zernike aberration coefficient. The lenses were fitted on three normal subjects (total three eyes). Wavefront aberrometry was performed pre- (naked eyes) and post- fitting.
Results: Regarding SA, modulation of the aberration was achieved in a consistent fashion towards the same polarity of the aberration, ranging from ~60% to +200% of the intended change. Regarding coma, lenses that employed coma of the same sign with the subject's coma, increased the coma of the eye-lens combination. Lenses with opposite coma than the ocular coma decreased the on-eye aberration coma, and even reversed it.
Conclusion: Modulation of on-eye spherical aberration and coma in a predictable manner employing custom-designed hydrogel lenses was achieved in normal eyes. Such lenses can be very useful in normal eyes with subtle high-order aberrations. Wavefront correction dispensing can be personalized, based on the design of customized contact lenses.
Keywords: Soft contact lens; Hydrogel contact lens; Wave front customized contact lenses; Wavefront aberration; Zernike aberration; Keratoconus; Irregular cornea; Keratoplasty; Irregular astigmatism; Asphericity
Introduction
The correction of high-order aberrations is a long-sought target in vision research. Through studies of ocular aberrations have demonstrated that most eyes exhibit low to moderate amounts of high order aberrations (HOA) [1-6]. Normal, healthy eyes, such high-order aberrations associated with the anterior cornea are partially-compensated by the aberrations (due to their opposite sign) of the intraocular optics such as the crystalline lens [7].
Hydrogel (soft) contact lenses (CL) are typically used in normal eyes, but their effect in restoring significant, non- rotationally symmetric aberrations is limited. Hydrogel CLs for such irregular corneas exist, but they do not achieve satisfactory corrected-distance visual acuity (CDVA) results in such eyes [8]. Another drawback of the existing CLs is that in order to mask aberrations, conventional CLs employ an increased lens thickness which results in a reduced oxygen permeability [9].
In the quest for improved vision restoration and comfort in normal eyes with some amounts of HOA, we propose soft CLs that employ custom HOA correction. These lenses should be of regular thickness; the correction can be implemented in the front lens surface, while the back surface is designed to aim for the clinically optimal fit. Alternatively, the correction can be implemented on the back lens surface, which theoretically will lead to a better fitting, especially in slightly distorted corneas. As many aberrations are not rotationally-symmetrical, the optical zone of such a lens should have a non-uniform thickness in order to achieve the desired correction, dependent on the amount of aberrations to be corrected and on the optical zone.
Our team has previously demonstrated [10] that wave front-customized soft contact lenses implementing correction of vertical coma improve visual performance in eyes affected with mild or moderate keratoconus. Optical quality and visual performance with such customized soft contact lenses for keratoconus eyes has been also proven efficient by other investigators [11,12]. The purpose of this study is to measure the effect of hydrogel CLs incorporating SA and coma in normal, healthy eyes in modulating such ocular aberrations. We seek, in other words, to demonstrate the feasibility of modulating HOAs in a controlled fashion. This will have a significant impact in wave front customized hydrogel CL design, as modulation of CL asphericity may be among the key factors in order to achieve management of presbyopia correction with contact lenses [13].
To this purpose, we designed and manufactured two types of customized contact lenses, and studied their on-eye performance. The first type implemented an anterior surface design with (fourth-order Zernike) spherical aberration (SA), the second type implemented (third-order Zernike) coma design. The reason we chose fourth-order SA and third-order coma as targets is that these aberrations are the main degraders of retinal image quality and visual performance, amongst all HOAs [14-16].
Methods
Design and fabrication
A computerized numerically controlled (CNC) lathe (Optheq, Contamac, UK) and the accompanying software (Calculens v.2.7, Contamac, UK) were employed to implement the custom design and fabrication. All lenses incorporated the designed HOA correction on the anterior surface. Each lens was designed to have only one non-zero Zernike aberration coefficient. Notation of SA and coma is according to the ANSI standards [17]. The lenses were designed and fabricated to have a certain type and amount of HO aberration over a 3.5mm pupil diameter.
The first type of lenses included a lens with positive 4th order SA (referred to as Sph+0.200), and three lenses with negative SA (referred to as Sph-0.030, Sph-0.100, and Sph- 0.150, respectively). The above numbers indicate the amount of spherical aberration (in |im root-mean-square RMS) implemented in the design. The second type of lenses employed 3rd order coma aberration as follows: the first lens (referred to as X-0.100) employed negative horizontal coma, and thus the orientation of coma was perpendicular to the lens stabilization modality (in these lenses, a prism ballast). The second lens employed negative vertical coma (referred to as Y-0.070) and the third lens (referred to as Y+0.150) employed positive vertical coma. The numbers again indicate the amount of coma in |im RMS implemented in the design. All of the lenses (total: 7) were of 8.4mm base curve, 14.5mm total diameter, 3.5mm optical zone diameter for the sphero cylindrical correction. The material was GM3 49% (Contamac, UK), which has 49% water content and a Dk value of 15.9. Central lens thickness was 0.12mm. After lathing, the lenses were properly hydrated. The design parameters were verified with a Clear wave Contact Lens Precision Aberrometer (Wavefront Sciences-now Abbott Medical Optics, USA), and a Rotlex Contest Plus lens analyzer (Rotlex, Israel). The Rotlex analyzer operates on the principle of Moire deflectometry [18], and outputs data in diopter format.
Lens fitting and measurements
Prior to the measurements with the wave front-guided lenses, informed consent was obtained from all three volunteer subjects. The lenses were fitted on the right eye of each subject. Each subject wore every custom lens. Prior to measurements, the fit of the lenses was checked in a slit lamp, to ensure that it fell within acceptable clinical standards [19]. Moreover, regarding the lenses employing coma, which employed a prism-ballasted stabilization method, it was also verified that lens orientation did not exceed 5 degrees. Lighting in the examination room was controlled, in order to avoid excessive dilation of the subject's pupil, beyond the 3.5mm optical zone of the lenses. No other measurement or estimation of lens misalignment, either rotation or translation, was performed on this stage.
Three consecutive measurements were taken and averaged with each of these lenses, with the COAS Wave front analyzer (Complete Ophthalmic Analysis System, Wave front Sciences, now Abbott medical Optics- USA). The COAS uses the Scheiner- Hartmann-Shack principle [20], which is embodied in a variety of clinical instruments, and its effectively in clinical use is documented by the peer-reviewed literature [21]. We performed the above measurements in order to ensure that any change in SA or coma of the wave front lens-eye combination was due to the customized lenses. As baseline reference measurements (also three consecutive) we used those of the naked eyes to be tested, without any lenses worn. After data collection, the Zernike aberration coefficients were computed for a 3.5mm pupil size employing the COAS' software.
Results
The spherical aberration of the eye of subject 1 was positive (0.012|im RMS), and moved to even more positive values with the Sph0.200 lens worn. When the lenses employing negative spherical aberration were worn, spherical aberration moved to more negative values. Similar results were observed for subjects 2 and 3. The spherical aberration of the right eye of subject 2 was 0.023|im RMS and moved to more positive values when the plano lens and the Rx lens were worn. The results for all lenses are presented in (Table 1-3). With the Sph+0.200 lens that introduced positive spherical aberration, the on-eye result in all patients became even more positive, whereas it became progressively more negative with the lenses implementing negative spherical aberration. It is, therefore, obvious that the lenses fit on all subjects, had the desired effect of changing the spherical aberration to the desired direction, and the change was quite proportional to the spherical aberration of the lens. considerably between subjects, as the Sph+0.200 lens induced However, there was considerable inter-subject variability 51%, 83%, and 42% spherical aberration than intended to of the effect, as reported in (Tables 1-3). This change varied subjects 1,2 and 3, respectively.

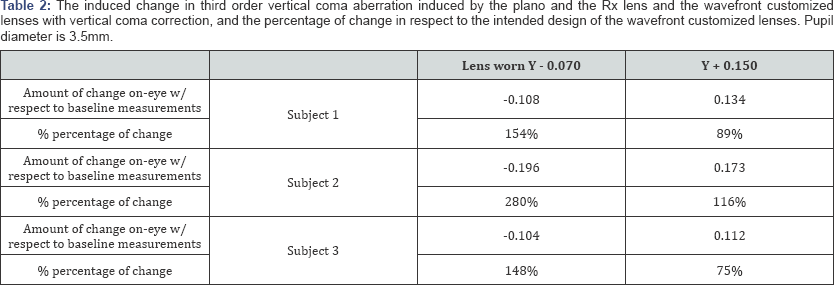
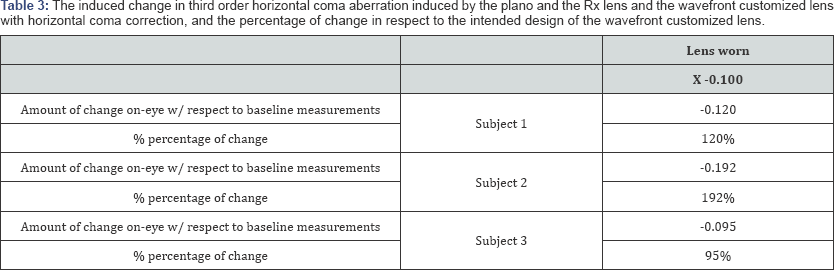
The results presented in Table 3 for the coma-implementing lenses bear similarity to those from the spherical aberration- implementing. The lens whose off eye aberrations was closer to the intended design, the Y -0.070 lens, had also variable effect in the three subjects' eyes, as it induced ~150% more negative coma than intended in subjects 1 & 3, and induced a 280% more coma in subject #2.
Discussion
The design and fabrication of wave front-customized lenses in both healthy and abnormal eyes has been demonstrated by Lopez-Gil et al. [22], where three groups, namely normal, keratoconic and post-keratoplasty, were evaluated for the effects of customized lenses on total and high-order aberrations. They found that wavefront-customized lenses reduced total aberrations on all three categories, but reduced HOA only in the keratoconic group. They attributed this to better stability of the customized lenses on the keratoconic corneas, whereas increased translation and rotation on the normal and postkeratoplasty corneas caused an increase of HOA. Regarding irregular eyes, Marsack et al. [23] designed, fabricated, and fitted a customized, lathe-cut contact lens in one eye of a keratoconus patient. This lens was found to significantly reduce HOA in the keratoconic eye, and consequently, improve vision. Sabesan et al. [24], followed the same procedure on a population of keratoconic eyes, and additionally compensated for decentration and rotation. They found that their customized lenses improved vision compared to a conventional soft lens and an RGP lens. Chen et al. [25], also fitted a group of keratoconic eyes with posterior-surface customized hydrogel contact lenses. These lenses were produced by sculpting the back surface with an excimer laser, in order to improve conformance of the lens to the cornea. These lenses created an overcorrection of ocular aberrations, due to the aberrations of the internal optics of the eye being revealed. To the best of our knowledge, there has not been so far a study of different types of wavefront-customized hydrogel contact lenses, targeted to one HOA mode each, and with various aberration magnitudes, in order to observe and measure the results on normal, healthy eyes. Such lenses, combined with the appropriate sphero cylindrical power, can be used to correct subtle HOA in normal healthy eyes and maximize visual performance, and in certain cases might even result in vision better than 20/20 [26,27]. Other cases that can benefit from wavefront-customized lenses with subtle HOA, are ones with small amounts of coma, such as sub-clinical keratoconus or mild irregular astigmatism.
The mathematical process of designing a wavefront correction in a hydrogel CL has been reported by Almeida et al. [28]. If correction of spherical aberration (SA) is desired, such as in the majority of normal eyes, or in cases of post-refractive surgery with small ablation zones or in central keratoconus, there should be a large radial symmetrical variation in lens power, from the lens center to the periphery up to the edge of the optical zone. This was the path followed by Dietze et al. [29,30], who designed and fitted on myopes and hyperopes a series of SA-correcting hydrogel CLs with spherical power, based on aberrometry data. They found that these lenses reduced SA, but increased total HO aberrations and did not improve vision compared to spectacles, regular spherical hydrogel CLs, or CLs designed to be aberration-free in air. They attributed this to the amount of uncorrected astigmatism, which in their study had a mean value of -0.50dpt, as the blur that it could cause on image quality surpassed the benefit of correcting SA, and to the small effect that such minor amounts of SA found in normal eyes. They concluded that normal subjects might benefit from such lenses in low-light conditions, where natural pupil dilation occurs and the corresponding SA is increased.
If coma reduction is the desired target, as in paracentral keratoconus, inside the optical zone of the lens there should be a coma-like pattern of refractive power, with the portion with the reduced refractive power located opposite to the cone, and the portion with the increased refractive power located against the rest of the cornea, covering the pupil. The latter modality obviously needs lens stabilization methods, in order to achieve proper orientation on the cornea and avoid lens rotation. The design of such lenses for HOA demands sophisticated lens design, and in the manufacturing process, a CNC lathe or an ablating laser should be used. Also, advanced optical quality setup is needed to measure the shape and verify the functionality of such lenses, as the simple (universally used) focimeter and the radiuscope are not sufficient enough. This study demonstrates the concept that wavefront-customized hydrogel contact lenses can be used for the manipulation and correction of ocular coma and spherical aberration in normal eyes. The results show that hydrogel lenses can modulate the Zernike aberration coefficients of the lens-eye combination, and specifically, coma and spherical aberration. The modulation can be predictable, to an extent beyond that possible with standard hydrogel contact lenses. It can be concluded that such lenses can be utilized in a clinical practice for providing custom wavefront vision correction. As the main reason of retinal image degradation, beyond sphero cylindrical errors, are SA and coma, we targeted these particular aberrations for designing and fitting wavefront customized hydrogel contact lenses.
It is well-known that once fitted properly, a hydrogel contact lens conforms to the corneal surface, in a manner which depends on the corneal topography, the geometry and the design of the lens, the material of the lens and the interaction with the tears. In a study by Jiang et al. [31], it was found that different types of hydrogel CLs alter the wavefront profile of the eye in a manner that differed considerably from one lens type to another. They hypothesized that this can be attributed to the optical quality and the design of the lenses, the lens centration, the tear film quality and the level of deformation of the lenses on the cornea. Also, Lu et al. [32], found in their study that hydrogel CLs had a trend towards inducing HOAs when worn. However, more research is warranted in order to investigate the alteration in the shape of wavefront-customized contact lens surfaces, anterior or posterior, when worn on the eye, as they might not have a uniform thickness, and deformation will affect visual performance.
Our results support the above hypothesis. The wavefront- customized lenses had different effects on the subjects' eyes, regarding the change of the magnitude of the targeted aberrations. This can be attributed to variable levels of lens deformation on the corneas of the subjects, which itself depends on corneal topography, lens design, tear film quality (which, along with micro-differences in the fit between the two subjects, might lead to variable patterns of lens dehydration), and lens translation and rotation.
The other major factors that affect the on-eye results of such lenses are rotation and decentration. We did not include calculations of coefficient transformation based on lens rotation and translation, as we wanted to test the hypothesis that wavefront dispensing can be performed without the tedious measurements and mathematical procedure associated with the above. However, we ensured that the fitting was at least clinically acceptable, which means that the lens was well-centered, and did not rotate more than 5 degrees or decentered more than 1-mm on blink. De Brabander et al. [19], have demonstrated through simulations that these criteria are more that acceptable for obtaining a benefit from a wavefront correction. Based on the results of our study, we believe that this hypothesis is valid, but the dispensing procedure might need to be further personalized and customized.
Cox et al. [33], have already described and patented [34], a process of wavefront dispensing. They stated that dispensing should begin with the fitting of a trial lens with macro parameters (thickness, base curve, diameter, sphero cylindrical power) as close as possible to the final wavefront lens. The correct clinical fit should be verified, and then the rotation and decentration of the lens should be recorded, and new wavefront measurements should be taken with the lens in situ. Lastly, the wavefront customized lens is designed based on the on-eye aberration pattern and the lens rotation and translation.
We believe that this procedure can be simplified by omitting the measurements of lens position and rotation. Guirao et al. [35], report a computational method for estimating the correction by taking into account translation and rotation. However, in another study which utilized an adaptive optics (AO) system [36], it is reported that the lens rotation and decentration normally found in practice (and which are clinically acceptable) still produce better visual results compared to conventional, non-wavefront customized contact lenses. The same results were found in another theoretical study by the same authors, which employed computations of the performance of an ideal wavefront CL after decentrations and rotations [37]. Based on our work and the studies described above [35-37] the authors believe that wavefront CL dispensing can be performed in the standard clinical practice, employing the current clinical standards of a good clinical fit, omitting the steps of measuring the lens position and rotation and recalculation of the coefficients. However, if the desired result is not achieved, due to lens rotation, decentration, deformation or all of the above, the new step that has to be added is the calculation and order of a new wavefront customized hydrogel CL.
The amount of aberration implemented on the new lens should depend on the amount of the first wavefront lens and the amount of change that it induced to the targeted aberration or aberrations. Alternatively, in order to avoid excessive reordering, the practitioner may have at his disposal a series of trial wavefront customized hydrogel CLs, with predetermined amounts of certain aberrations in multiple magnitudes. He should then choose the first lens based on the aberrometer results, fit the lens, re-measure the on-eye aberrations and over-refract, and order the final lens with increased confidence. Even then, the expected result might not be fully achieved, mainly due to different patterns of deformation of the two slightly different lens geometries on the cornea. This difficulty might be larger in normal eyes which nevertheless have minor amounts of HOA, due to the instability of HOA over time [6], and to fluctuations caused by accommodation [38].
Various studies have already demonstrated, both theoretically and in a clinical setting, the feasibility of a custom wavefront hydrogel CL correction in abnormal eyes, and also investigated the required extent (in Zernike orders) of such a correction. As mentioned above, such eyes present with large amounts of HOAs, mainly coma and spherical aberration. In addition to abnormal cases, patients who present with mild amounts of coma, trefoil, and related high order aberrations can also benefit from this technology. Cases with small amounts of coma include sub clinical (form fruste) keratoconus, and mildly asymmetrical corneas. Maximizing visual performance in such eyes requires correction for the majority of the above aberrations. In specific, spherical aberration management wavefront lenses can be of great value both in normal eyes, with small to moderate amounts of spherical aberration, and also to cases such as central keratoconus or post-refractive surgery corneas, with small ablation zones over a large pupil. Correction of spherical aberration in the former is supposed to maximize visual acuity and hypothetically lead to supernormal visual performance, although previous studies did not succeed to increase acuity with the use of such lenses. In the latter is expected to restore vision, especially in medium and low contrast environments and in mesopic or scotopic levels of lighting [39] where large amounts of spherical aberration lead to the subjective impression of halos and blur circles.
Trefoil, tetrafoil, and related aberrations that are positioned near the edges of the Zernike pyramid are considered to have less impact in vision that aberrations near the center of the Zernike pyramid, if the same amount of RMS error is considered [23]. However, patients who have undergone penetrating keratoplasty often present with a substantial amount of such aberrations due to variable suture tension [40], and the study of Marsack et al. [41], implied that these aberrations should also be corrected in keratoconus eyes. The perceptual ability of each individual should be taken into account when designing a wavefront correction. When a person reads a visual acuity chart, he translates the PSF at the retina (formed by the eye's optics) into familiar words or numbers. This PSF is unique to each individual, and its basic shape remains basically unchanged through age. There are two possibilities when correcting most of the eye's high order aberrations. The first is to reduce the total RMS error (as measured by an aberrometer) and increase the Strehl ratio, but at the same alter the shape and/or direction of the PSF on the subject's retina. For example, one could slightly overcorrect a large amount of coma and change its sign from positive to negative or vice versa, and at the same time, the total RMS error could be less than the previous uncorrected state and the Strehl ratio increased. The second possibility is to reduce the RMS error and not alter the shape of the PSF. In the above example, this can be achieved by carefully avoiding overcorrection of coma. If this can be achieved, the total RMS error is reduced, the Strehl ratio increased, and the shape and the direction of the PSF remain basically the same.
If by employing a wavefront correction the first scenario is realized, it is possible that the person will lose corrected- vision lines, despite seeing through better optics, as he is not accustomed to translating the new image shape in his retina. In a study by Artal et al. [42], it was discovered with the help of AO, that subjects had a sharper impression of a certain stimulus when they viewed it with their own aberrations, than with a rotated version of their aberration pattern. In a consequent study, Chen et al. [43], found that the best subjective image quality did not coincide with the best possible retinal image quality, and neural adaptation occurred, although the 'intensity' or duration of this phenomenon was not investigated. Other studies [44,45] have found that perceptual adaptation to myopic blur occurs to both myopic and emmetropic subjects, and both grating and letter acuity improved after a period of exposure to myopic defocus. Thus there is a risk of reducing visual acuity associated when dispensing wavefront guided contact lenses, although if the wavefront guided correction provides better vision at the time of the initial fit, this risk is considered minimized.
Conclusion
This study demonstrates that wavefront-customized hydrogel contact lenses can be used for the modulation and correction of spherical aberration and coma and in normal eyes. The results show that wavefront-customized hydrogel CLs can change the Zernike aberration pattern of the lens-eye combination, and specifically, spherical aberration and coma, in a predictable fashion. Such lenses may be utilized in a clinical practice for providing custom wavefront vision correction in both normal and abnormal eyes, by following the current clinical standards of a good fit. However, as the effect of a customized CL with a predetermined amount of aberrations differs from eye to eye, in the presence of residual aberrations new lenses can be designed, based on the change in aberrations imposed by the first ones. Larger studies need to be undertaken, in order to test the large-scale feasibility of such a procedure, as there is a considerable contribution of the neural factor in visual performance. If, however, such a method can be found to be reliable, it would greatly simplify wavefront dispensing for the everyday clinical practice.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com/index.php
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment