JUNIPER PUBLISHERS- JOJ Ophthalmology
Abstract
Objective: To investigate possible effect of
eplerenon 50 mg in serous pigment epithelial detachment (sPED) and
subretinal fluid (SF) resolution after initial intravitreal application
of 2 mg aflibercept in treatment of neovascular age-related macular
degeneration (nAMD).
Method: Case presentation of two females with
occult choroidal neovascularisation with sPED due to the nAMD treated
with three consecutive intravitreal injections of 2 mg aflibercept. On
control check up 6 weeks after last injection, per oral 50 mg Eplerenon
(Inspra) once daily is prescribed. For follow up we used visual acuity,
intraocular pressure, Amsler grid test, color fundus (CF), optical
coherence tomography (SD OCT) baseline, 6 weeks after last intravitreal
injections, 6 weeks after initiation of eplerenon as well as potassium
serum concentration 6 weeks after initiation of eplerenon therapy is
monitored.
Results: Morphologic improvement evident in
reduction of central macular thickness and height of sPED >10%
followed with stabile visual acuity was registered in both patients
after 6 weeks of eplerenon prescription.
Conclusion: Eplerenon given as adjunctive
therapy for treatment of sPED in nAMD could have beneficial effect but
further more detailed and more controlled clinical investigations are
recommended.
Keywords: Serous pigment epithelial detachment; Eplerenon; Neovascular age related macular degenerationIntroduction
Serous pigment epithelial retinal detachment (sPED)
is sharply demarcated, smooth, dome shaped elevation of retinal pigment
epithelium (RPE) [1].
SPEDs are manifestation of neovascular age related macular degeneration
(nAMD), polypoidal choroidal vasculopathy (PCV) and central serous
chorioretinopathy (CSR). Controversy remains about etiology of sPEDs [2-5].
The over activation of the mineralocorticoid receptor (MR) pathway has
been shown to cause fluid accumulation in the retina, choroidal
vasodilation, and to promote retinal neovascularization in hypoxic
conditions [1-4,6-8]. According the role of mineralcorticosteroid receptors in retina, eplerenon has shown beneficial effect in treatment of CSR [5].
A well-known complication of PED is a RPE tear caused
by contraction of the elevated PED and retraction of RPE resulting in
absence of RPE underneath the neurosensory retina [5,6].
RPE rip could be serious vision threating complication of laser
photocoagulation, photodynamic therapy and anti-VEGF therapy. There is
an evidence that sPED with height > 350 ?m are more high risk for
development of RPE and consecutive macular atrophy [7].
Anti VEGF is nowdays the main therapeutic approach for nAMD and despite
chronic presence of sPED and subretinal fluid in regular and continuous
anti-VEGF regimes have comparable and benefitial effect in visual and
functional outcome [8].
Due to the costs of antiVEGF and patient compliance with intravitreal
injections alternative treatments are rational approach to those cases [5].
Case Presentation
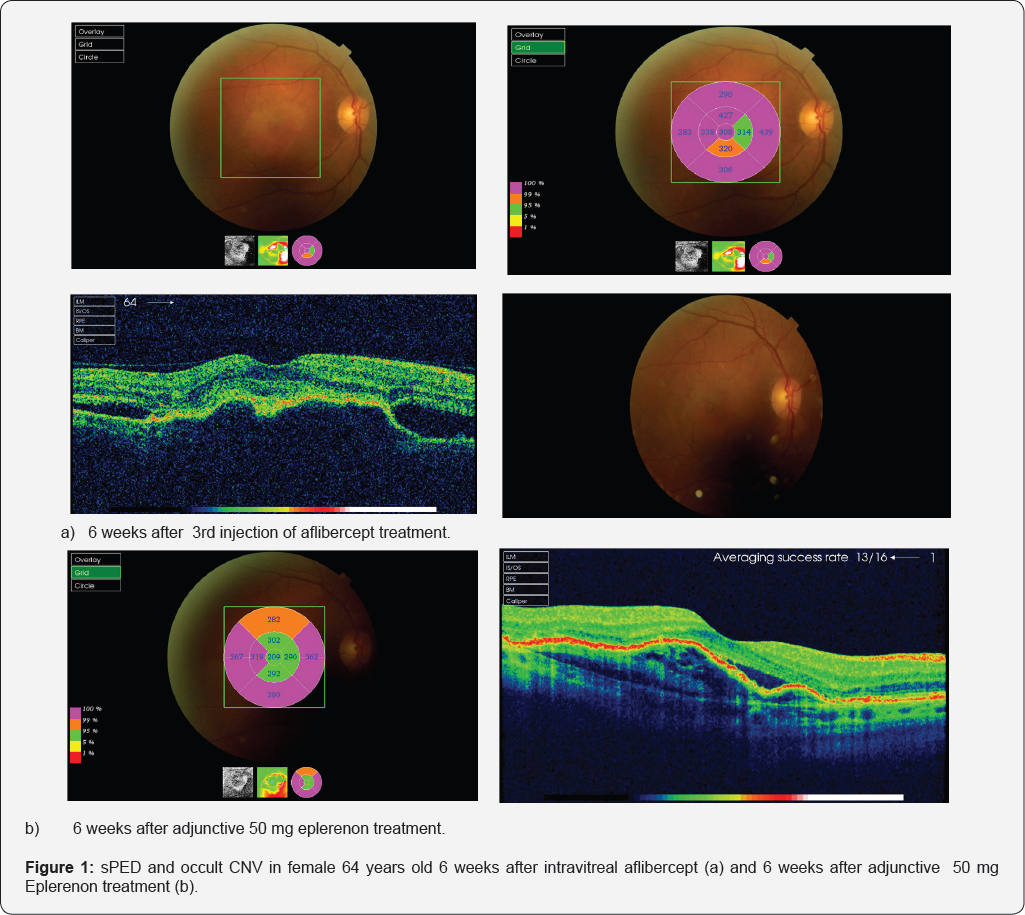
Case series of 2 patients with occult choroidal
neovascularisation (CNV) due to the nAMD with sPED >350 чm,treated
with three initially consecutive intravitreal injections of 2 mg
aflibercept (EYLEA®) in private practice. After 6 weeks after last
intravitreal aflibercept therapy per oral Eplerenon 50 mg (INSPRA®) once
daily was prescribed as persistent sPED exists and relatively large
collection of subretinal fluid (>50 чm) presented in macular region.
Both patients are females, age of 71 and 64. Visual acuity baseline 30
ETDRS (Early treatement diabetic retinopathy) letters.
After 12 weeks of last treatment with anti VEGF and 6
weeks after Eplerenon prescription visual acuity was 70 and 75 ETDRS
letters respectively. Intraocular pressure was with normal limits during
all controls (less than 21 mmHg). Both patients had detailed
ophthalomologic examination on all consecutive visits. It included
complete anterior segment of the eye exam which was within normal limits
in both cases. Fundoscopic exam in mydriatic conditions show soft
drusen on both eyes, complete resolution of the blood on eplerenon
baseline visit and no blood on consecutive visit in treated eye. Both
patients had incomplete posterior vitreous detachment, no vitreoretinal
changes. Fellow eye has high risk AMD in younger patient (presence of
large soft drusen in macula). In other patient fellow eye has soft
drusen and occult juxtafoveal CNV. Both patient were treatment naive.
Both patients were previously for 5 years treated
with oral beta blockers (metoprolol 25 mg once daily) and ACE inhibitors
(enalapril 10 mg twice daily) for arterial hypertension and received
statins (atorvastatin 10 mg once daily) for regulation of
hyperlipoproteinemia type IIa. Other systemic and ocular health problems
were not present. Both patients presented type A personality. Central
retinal thickness and central sPED height measured 6 weeks after
eplerenon 50 mg treatment and 12 weeks after last intravitreal injection
of 2 mg aflibercept seemed to be evidently reduced. Visual acuity
during treatment with eplerenon 50 mg was stable through 6 weeks 70 and
75 ETDRS letters respectively. Both patients are educated for self
testing Amsler grid, and Amsler grid tests performance was stable and
unchanged during all follow up period. Potassium plasma level was
monthly monitored in both patients (within normal limits <4,1
mmol/L). Younger patient is now switched to pro re nata (PRN) anti VEGF
therapeutic regime, as signs of CNV activity in both cases considered
are visual acuity, Amsler grid test, signs of hemorrhage on clinical
exam, increase in retinal thickness due to the intraretinal edema on OCT
(Figure 1).
Other patient refuse further antiVEGF treatment and she is still taking
eplerenon combined with antioxidant and vitamin supplements.
Discussion
The purpose of this case presentation is to show
effect of eplerenone, a mineralocorticoid receptor antagonist, as a
treatment option for reduction of SRF and sPED in cases with nAMD. The
role of mineral corticosteroid receptors (MR) in retinal disorders is
emerging and the potential association with physiological traits are
investigated in CNV. The place of MR antagonists for retinal diseases
treatment are discussed [1-4].
Central subfield thickness at follow-up visit after
eplerenon initiation significantly decreased more than 10% from baseline
which was previously reported in cases with chronic CSR [5].
Following therapy with eplerenon, there was a significant reduction in
SF, reduction in CST, and improvement visual acuity in eyes with chronic
CSR [5]. A majority of eyes with CSR presented by Singh and al [5]
(47.1%) demonstrated stable SRF on treatment, while 35.3% had complete
resolution of SRF. Results of this study indicate that eplerenone could
be beneficial in the treatment of unresolved CSR. Considering that some
cases in nAMD morphologically reminds on CSR could be rational approach
to treat those patients with mineralcorticosteroid antagonists with the
goal of serous transudation reduction and to reduce number of
intravitreal injections which could be serious burden for patients.
Also, presence of subretinal and sub RPE fluid is still not mandatory
indication for continuous and strict anti VEGF regime. There are
evidences that antiVEGF therapy in cases with large serous PED are prone
to RPE rip [7,8].
As it is still controversial, there could be some benefit of
anatgonists of mineralcorticosteroid receptors in some cases with
resistent and non compliant patients with sPED. Further more precise
conclusions and role of mineralcorticosteroid receptors in nAMD request
more controlled and precise clinical investigations.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment