Juniper Publishers-Journal of Ophthalmology
Abstract
The Ciliary body is an unusual location of uveal
melanomas and usually these kinds of tumors appear with a reduction of
vision due to the formation of sectorial cataract or retinal detachment
when the tumor spread to a posterior position. We present a 57 years old
woman with sudden and severe ocular pain. Ophthalmologic examination
showed a hyper mature cataract and superior displacement of the lens
with sectorial angular block. The intraocular pressure was 22 mmHg.
After papillary dilation aciliary body tumor was observed. The
ultrasound study and magnetic resonance imaging confirmed the diagnosis
of uveal melanoma.
Background Information:during
the years 1991-2015, about 54,000 consecutive cases were examined at the
ophthalmic out patient’s clinic. The aim of this study was to find out
if any relationship exists between aging disorders, or each is having
its own entity, or one disorder could be the driving factor to produce
aging and related complications.
Methods:Findings were entered
into computerized documentation program that does simultaneous analysis
of clinical data. The correlation between aging disorders was analyzed.
Results:Seven disorders were
found to be related to aging; hypertension, glaucoma, cataract,
diabetes, age related macular degeneration and ischemic neuropathy, in
addition to presbyopia. Hypertension was found to be the leading cause
for the development of ischemia and therefore may be the stimulating
factor for the development of oxidative stress and oxidation. It shows
that basic trends of aging are important while investigating the
metabolic disorders at molecular level.
Conclusion:Taking both factors;
ischemia and oxidative stress into consideration, it is recommended a
strategy be adopted, in addition to antioxidant therapy, prophylaxis and
prevention of aging includes medication that guarantees healthy
relationship between hypertension and cerebral blood flow.
Keywords: Aging disorders; Diabetes; Hypertension; Cataract; Glaucoma; Age related macular degenerationIntroduction
During the years 1991 and 2015, about 54 000
consecutive cases were examined at the Ophthalmic Clinic in Amman -
Jordan. Data were entered directly into a computerized documentation
program that performs simultaneous analysis of clinical data. Figure 1
shows the age distribution of examined cases. One notices that Jordan
has a relatively young population and a significant decrease of
incidence starting at the age group 61-70 years.

It has been noticed that seven diseases increase with
age; Hypertension, Diabetes, Glaucoma, Cataract, Age related Macular
Degeneration “AMD” and Ischemic Neuropathy, in addition to Presbyopia.
The question that arises, is there any relationship between these six
disorders? Or each is having its own entity independent of each other?
Or one disorder could be the driving factor to produce aging related
complications within the other components?
Materials
The age distribution of examined cases is shown in
Table 1. A comparison between aging subjects to all examined cases
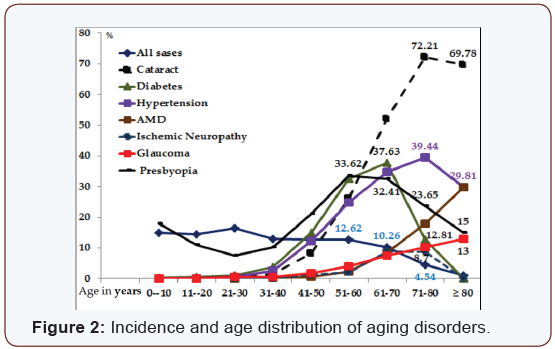
(Figure 2) gives us the following information;
- The incidence of aging for all disorders starts to increase at the age of 40 years.
- Diabetic cases start to decline at the age 61-70 years.
- Cataract and hypertension starts to decrease at the age group of 71-80 years.
- Open-angle glaucoma and AMD continue to increase until the age of 80 years and above.
- The accommodative reservoir decreases from birth up to the age of 30 years and Presbyopia starts to develop in average at age 40 and continues to increase up to the age 61- 70 years.

As the incidence of all disorders start to increase at age 40
years, means that the age of 40 is the starting point of aging. This
fact could be confirmed as presbyopia starts in average at the
age of 40 years. It is possible that the decline of aging incidence
(Figure 2) after the age of 61- 70 years by diabetics and at the
age of 71-80 years by cataract and hypertension means a relative
early death for these two diseases as compared with the normal
distribution of all cases with in the same age group.
Cataract
Cataract increases with age, reaching its maximum 72.21%
at the age of 71- ≥ 80 years. Its incidence with age is much
higher than all other disorders. “Implications of oxidative stress
have been examined in the pathogenesis of cataract in vivo
treatment with vitamin E, of the Emory mouse led to a decrease
in the rate of cataract progression suggesting that in at least
in some entrances an oxidative stress could participate in the
formation of cataract [1]. It is known that in addition to heredity,
environmental factors play a major role in the development of
cataract. In addition, 35.5% of all cataract cases are diabetics,
34% hypertensive, 10.6% have AMD and 8.6% Glaucoma. So cataract is involved in a mixture of additional components that
might affect its development and patient’s quality of life. It is
therefore expected that cataract patients are also affected from
ischemic disorders in the same manner like other aging diseases.
Hypertension
Hypertension increases with age reaching its maximum
39.44% at the age 71-80 years, and then it decreases again. It
is known that uncontrolled hypertension causes hypertensive
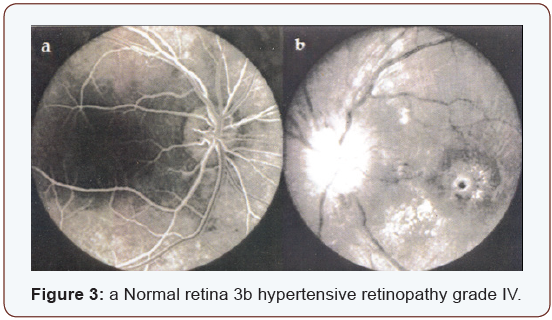
retinopathy. According to its severity, hypertension is classified
into four grades (Figure 3) a represents a normal retina.
The ratio of diameter between venules and arterioles is
3:2. (Figure 3) represents hypertensive retinopathy grade IV,
showing narrowing of the arterioles, and swelling of the optic
nerve head, macular edema, micro hemorrhages and cotton
wool spots indicating the presence of severe ischemia. Wayne [2]
says “There is increasing evidence that atherosclerosis should
be viewed fundamentally as an inflammatory disease. There is
evidence that hypertension may also exert oxidative stress on
the arterial wall”.
Diabetes
Diabetes increases gradually with age. It reaches the
maximum incidence “37.63%” at the age 61-70 years. Its
distribution goes parallel to hypertension with the difference
that diabetes starts to decline earlier as seen in (Figure 2).
There is convincing experimental and clinical evidence that
the generation of reactive oxygen species increases in both
types of diabetes and the onset of diabetes is closely associated
with oxidative stress Some [3] diabetic patient care severely
affected with uncontrolled hypertension and the development
of hypertensive retinopathy and other vascular disorders in
comparison to non-diabetics (Figure 3).
It is expected that diabetic patients with severe hypertension
most likely suffer from decreased cerebral blood flow and
ischemia of sensitive organs, with the result of getting ischemic
neuropathy and renal failure or different vascular obstructions.
Similar to hypertension, the prevalence of glaucoma by diabetic
patients is 7.7%, much higher than by all examined patients
“2.28%”.
Glaucoma
Open angle glaucoma increases with age, starting at the age
of 40 years and reaching its maximum “13%” at the age of 80
years. The blood pressure seems to be responsible for aqueous
humor formation [4]. The incidence of glaucoma among all
patients is 2.28%, and 6.6% among all hypertensive patients.
Matt [5] reports of having evidence that antioxidant treatment
could help defeat glaucoma. It was found that antioxidant
treatment reduces oxidative stress in pressure-treated retinal
ganglion cells. This confirms a study done by Weinreb [6] that
oxidative damage occurs within hours of elevated hydrostatic
pressure or elevated intra ocular pressure.
Age related macular degeneration
Age related Macular Degeneration “AMD” increases with
age reaching its maximum 29.81% at the age of ≥ 80 years. The
incidence of glaucoma among AMD patients is 6.32% much
higher than by all patients included in the study “2.28%” and
with hypertension 5.3 %. We experience today exactly what
Donders [7] has described Khan HA & Moorhead HB [8] has
published, Frank [9] 25 years later that among the four aging
blinding diseases, Cataract, Glaucoma, Diabetes and AMD, Agerelated
Macular Degeneration is the only one for which there are
no effective means of prevention or treatment.
Although it is less common loss of vision in AMD, choroid
Neovascularization leading to disc form degeneration produces
a more rapid and dramatic and more severe decrease in vision
than the atrophic or dry form of AMD. Similar changes were found
also among patients in cases of diabetes, AMD, disc form macular
degeneration and high myopia, where the clinical appearance
of an often round macular scar, that has been recognized to
comprise Neovascularization, arising from the chorio-capillaris
[10] and proliferative changes at optic nerve head in cases of
carotid thrombosis (Figure 4).

Discussion
Aging is a complex of degenerative changes starts at the age
of 40 years. Presbyopia is the first measurable sign of aging. The
age of 40 years is therefore considered as the starting point for
prophylaxis, prevention and rehabilitation in order prolong life
expectation and to secure better quality of life for elderly. The
presented data show clearly that oxidative stress and oxidative
damage initiated much interest by researcher. Oxidative stress
is most likely responsible for the ongoing development of
oxidative damage and its complications by all mentioned aging
diseases. The pathogeneses of these diseases at molecular level
gives better insight into a major problem related to aging; the
oxidative stress causes a continuous oxidative damage. By the
presence of aging diseases and absence of cure, it is expected
that prevention with antioxidants might improve or maintain
these disorders at acceptable level, but keep fighting to prevent
the ongoing oxidative stress is mandatory. Hypertension on the
other hand involves all aging diseases as seen in (Table 2).

Ophthalmo-dynamometry is a good method “at least for serial
investigations” to measure the blood pressure in both brachialand
ophthalmic artery, estimate the vascular resistance and
calculate the amount of cerebral blood flow [11] Values that are
higher than twice the standard deviation (2xD) of the regression
curve are considered as having high cerebrovascular resistance
(CVR). The Cerebral Blood Flow (CBF) will be calculated as
follows;

In addition to the genetic and environmental factors,
uncontrolled hypertension seems to play a leading role in the
development of complications related to aging diseases. 47.1%
of all hypertensive patients suffer from Glaucoma, and 92.5%
of all diabetics are hypertensive. The incidence of glaucoma in
hypertension is relatively high “6.6%” in comparison to 2.28% by
all examined cases; the incidence of hypertension by AMD patients
is 26.7%. As expected hypertension might cause embolism of
the central retinal artery CRA the increased vascular resistance
measured by ODM on the (Figure 5).Other side not affected, show
increased vascular resistance by 59% of all CRA embolism cases,
is an alarming sign that such ischemic changes might occur on
the other side or elsewhere in the body. Treatment with antihypertensive
drugs is important. The positive expected effect
of some anti-hypertensive drugs “decrease blood and intra–
ocular pressure” could unlikely elevate the cerebral-vascular
resistance and decrease the cerebral blood flow as experienced
with clonidine [12,13]. It is therefore expected that patients
involved within aging diseases suffer from complications related
to hypertension and/or a non-wished side-effect of some antihypertensive
drugs causing ischemia. Hypertension seems to be
the leading and stimulating factor that causes arteriosclerosis,
increased vascular resistance and inability to maintain normal
blood flow to the whole body, causing severe damage especially
to the very sensitive organs, e.g. stroke, myocardial infarction,
gangrene, thrombosis and emboli of the central retina or carotid
arteries, ischemic neuropathy and renal failure. It might affect the chorio carcinoma and RPE causing ischemia. It is therefore
possible that oxidative stress which plays a major role at the
molecular level is initiated by ischemia. One comes in agreement
with Newell [14] that these macular changes are related to the
decreased blood flow of the chorio carcinoma below the fovea. If
this theory is correct, increased blood pressure and decreased
Blood flow will produce adequate systemic complications within
aging diseases. This could be confirmed by the presence of
associated disorders as shown in [Table 3] and (Figure 6 a and
b).

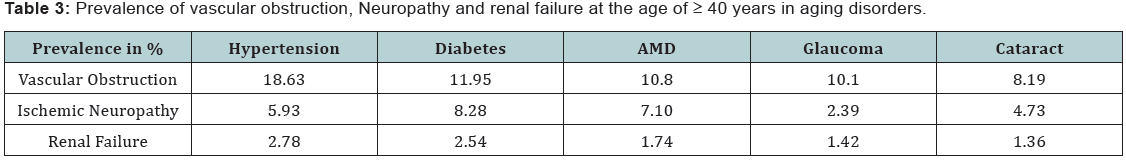
The majority of cases suffering from vascular obstruction
are found frequently in hypertension followed by diabetes, AMD,
glaucoma and cataract. Ischemic Neuropathy; “ischemic papillitis,
retro bulbar neuritis, and other cranial nerves” were found
most frequently by diabetics, followed by AMD, in association
with hypertension. By calculation the prevalence related to all
cases involved in the study, hypertension was found to be the
leading disease causing ischemic disorders; Diabetes increases
the prevalence of ischemic neuropathy and renal failure. By
observing the distribution curve (Figure 2 & 7) one comes to the
following life expectation and survival rate of aging diseases. By
considering all cases involved in the study independent of age,
the survival rate at age 51-60 years was found to be 12.7% and
for the age group ≥ 80 years 1.1%. As aging diseases starts to increase by the age of 40 years where the younger population is
excluded, it is expected that the survival rate for aging disorders
will be different. The prevalence of Cataract, AMD, glaucoma and
hypertension continue to increase till the age of 61-70 years.
Then the survival rate becomes less. The best survival rate for
the age group 71-80 years is for AMD 34.5%, followed by cataract
23.6%, then glaucoma 20.6%, hypertension 16.8% and diabetes
12.3%. The worst survival rate at the age of ≥ 80 years is for
diabetics 1.8% and the best was found to be for AMD patients
13.4%. The survival rate of the same aging group for glaucoma
6.1%, cataract 4.1% and hypertension 3% only.

Conclusion
The central regulation between systemic blood pressure
and cerebral blood flow is very important. Deregulation of
this mechanism through hypertension seems to be the leading
factor that initiates oxidant stress, oxidative damage and aging.
Antioxidants are therefore very important to prevent further
deterioration of aging disorders. For the prophylaxis of aging
diseases it is recommended that in addition to antioxidants,
special attention be paid to control hypertension and maintain
normal cerebral blood flow.
Highlights
Programmed computerized documentation and
analysis of aging disorders among 54000 ophthalmic cases.
Correlates between the most common seven aging
disorders in ophthalmology.
Demonstrates the importance of paying attention
to ischemic systemic disorders associated with ocular
complaints.
Modern eye Journals are not paying enough attention
to the basic trends of aging.
Suggests new strategy for the prevention of aging
disorders.
For more articles in JOJ Ophthalmology please click on:
https://juniperpublishers.com/jojo/index.php
https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment