Juniper Publishers-Journal of Ophthalmology
Abstract
Objective: To describe a
clinical case of external ophthalmomyiasis in a 55 year old man from
Umbria, Italy. We are also taking into consideration a differential
diagnosis of Onchocerciasis and Cisticercosis.
Design: Case Report Interventional
Participants:1 patient, 2 eyes in an interventional case report
Methods:biomicroscopic examination,
surgical removal of the larve, medical treatment, laboratory examination
of the specimen and blood screening
Main Outcome Measures:It was not
possible to obtain microscopic evidence of the larvae. Blood screening
and examination of the specimen was negative but the biomicroscopic
evidence of the parasites, together with documented information, made
the diagnosis relatively easy
Conclusions:The difference in
clinical signs and negative laboratory tests allowed us to exclude all
the diseases mentioned above. With case study, we hope to be able to aid
in simplifying the diagnosis of this pathology for our colleagues.
Keywords: Ocular Pain; Melanoma; Ciliary Body; CataractAbbreviations: BCVA: Best-Corrected Visual Acuity; NMR: Nuclear Magnetic Resonance
Introduction
Ophthalmomyiasis is an infection of the eye by
Diptera larvae. Oestrus Ovis is the most frequent cause of ocular
myiasis especially in countries with tropical or mild climates [1]. The
presence of this pathogen is widely seen in Central and Southern Italy
and the islands where sheep farming is common [2]. Ophthalmomyiasis,
based on its location, is classified as external, internal and/ or
orbital. In its external form the larvae are found on the conjunctiva or
on the edge of the eyelid [3]. With accidental contact this can give
rise to inflammation of the conjunctiva. The patient may also experience
lacrimation, photophobia and foreign body sensation in the eye.
Case History
55 year old male patient, telephoned from Umbria
where he was attending an open air public manifestation. He stated that,
whilst sitting under a tree the previous evening, he had the sensation
that something had “hit” his left eye. He complained of foreign body
sensation, pain and photophobia throughout the night. He was advised to
come to our private practice. At 14.00 h he arrived. His general
condition was good. His left eye was red, painful and intensely
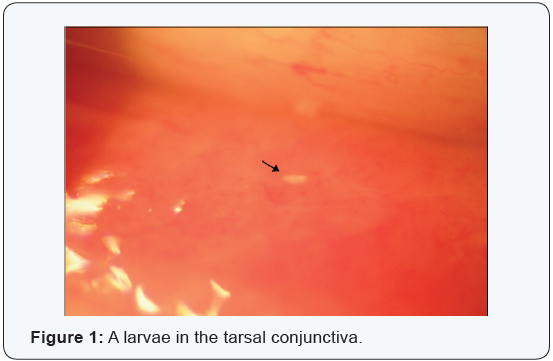
photophobic. A biomicroscopic examination revealed numerous tiny worms
in rapid movement (Figure 1). The worms were removed by using forceps,
cotton buds and continuous irrigation of the inferior and superior
conjunctival sac with a iodopovidone 5% solution and netilmycin sulphate
0.455g eye drops equal to 0300g. The patient was then treated with
netilmycin sulphate ointment every two hours. At 22.00 h after a second
biomicroscopic examination more larvae were removed. Some larvae were
preserved in test tubes containing tears and others were placed on
slides to be microscopically examined in the laboratory.
The specimens (slides and lacrimal liquid collected in tubes)
were examined immediately. One drop of physiological solution
at 0, 9% was added to the lacrimal fluid and placed on dry glass
slides and observed microscopically (first at 10x field and then
40x). No Diptera larvae were found, because they had dissolved.
Giemsa slides at 3% were prepared next. This stain is used to
highlight the visibility of other forms of parasites, particularly
nematodes and larvae of platelminta cestodes. Thin films of
lacrimal liquid were fixed with methanol and then stained with
Giemsa at 3% Microscopic examination, at 1000x with an oil
immersion lens revealed no parasites.
The following day a blood sample was drawn and
biomicroscopic examination revealed the presence of a few slow
moving larvae. These were removed with forceps. A complete and
thorough examination (vision, IOP, anterior chamber, vitreous
and fundus) was normal aside from conjunctival injection. An
examination two days later showed the presence of cysts situated
in the conjunctiva (Figure 2). The base of the cysts was pearl in
color but the upper part was transparent. Haemato chemical
tests were negative and a diagnosis of ophthalmomyiasis was
made based on physical evidence. An examination six days later
revealed a slight reduction in the size of the cysts and an absence
of larvae. After eight days the cysts were in a phase of regression
and the conjunctiva was no longer inflamed.

Discussions
The term myiasis means the invasion of human tissue by
parasites of the type Diptera. The first case of ocular myiasis
was described by Keyt in the 1900s [1]. The ocular form can be
external, internal or orbital and is commonly associated with
Oestrus Ovis [4]. Infestation occurs when the female lays her
eggs on the skin or mucous membrane. Stimulated by the warmth
these eggs evolve into larvae that are about 1.5 mm in size. The
larvae then penetrate the skin or mucous membrane in a few
minutes. Penetration inside the eye occurs from perforation of
the sclera which allows the larvae to move below the retina.
This may leave a hypopigmented trail. Entry into vitreous
chamber may occur due to a break in the retina. The larvae can
be trapped in the vitreous and gain entry into the anterior or
posterior chambers. The risk is partial dislocation or dislocation
of the lens and damage to suspensory ligaments (zonulules)
[5]. The signs and symptoms of internal ophthalmomyiasis vary
accordingly to anterior or posterior positioning of the larvae.
The signs of anterior positioning are recurring iritis associated
with partial displacement or total displacement of the lens. In
posterior positioning one can see vitreous turbidity and possible
detachment of the retina [6].
External opthalmomyasis presents symptoms similar to
acute catarrhal conjunctivitis as in the case presented. However
it is necessary to pay much attention to the treatment, because it
could have serious complications such as conjunctival ulceration,
endophtalmitis and invasion into other regions of the eye and
orbit [4]. Diagnosis is based on anamestetic and clinical data.
Identification of the parasite if it is microscopically present. The
typical parasitological aspects are, length a little over 1 mm, offwhite
color and two hooks in the cephalic segment. Examined
under a light the fissures appear tiny and fusiform with
cylindrical translucid elements and a black mark at one end. This
allows the parasite to be highly mobile and capable of penetrating
the conjunctiva [2]. Note, it is extremely difficult to remove and
preserve these larvae due to their fragility. Even though some
were rapidly placed on slides and others saved in lacrimal liquid
in the test tubes, it was not possible for the laboratory to examine
them as they dissolved. Treatment requires continual removal of
the larvae and antibiotics to prevent further bacterial infection.
We found that irrigation of the conjunctiva with a solution
of iodopovidone 5% and nethilmycina, did reduced the number
of larvae which helped lower the risk of further infection. It is
also necessary to be on the lookout for other conditions that
could occur due to larvae having entered the eye. We refer in
particular,to cysticercosis and onchocercosis, which , initially,
had been considered as possible differential diagnosis.
Cysticercosis is a parasitic disease caused by larvae
of
platelminta cestode of taenia type A. This cestode has man as
its final host and pigs are the intermediary hosts [7]. Clinical
symptoms depend on the site of infection and migration. One can
see conjunctivitis, iridocyclitis, displacement of the lens, retinal
detachment, vitritis, etc. Decreased vision, pain and foreign
body sensation are symptoms that the patient may experience
[8]. Diagnosis is made by looking for anti cysticercus serum
antibodies; enzyme linked immunoelectro transfer blot (EITB).
Onchocercosis is an infectious disease caused by infestation
of nematode filariform onchocerca volvulus. The incubation
period of 3-12 months shows no clinical signs [9]. The first sign
is usually the appearance of subcutaneous nodes. Lesions to the
eye, starting at the cornea, begin with opaque white infiltrates
and keratitis, followed by corneal opacities. Microfilarie found
in the anterior chamber can cause iridocyclitis and glaucoma,
whereas, regardless of microfilarie in the posterior chamber,
it is possible to find atrophied areas of the retina and choroid.
Involvement of the retina can lead to damage of the optic
nerve causing reduced vision or eventually blindness [10-11].
Diagnosis is made through anamnestic and laboratory data:
an increase in eosinophil, immunoenzymatic tests and the
presence of microfilarie. Sample is taken during the night when
reproduction of filarie is at its highest.
Conclusion
Although it was not possible to obtain microscopic evidence
of larvae, the symptoms, the biomicroscopic aspect of the
parasites, together with documented information, made the
diagnosis relatively easy. The difference in clinical signs and
negative laboratory tests allowed us to exclude any of the
diseases mentioned above. With case study, we hope to be able to
contribute and aid in simplifying the diagnosis of this pathology
for our colleagues.
For more articles in JOJ Ophthalmology please click on:
https://juniperpublishers.com/jojo/index.php
https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment