Juniper Publishers Ophthalmology is a progressive journal that presents the information concerned with the study and treatment of disorders and diseases of the eye. JOJO has worldwide distribution and supports medical professionals in the delivery of excellent ophthalmic information by publishing
Tuesday, 24 September 2019
Juniper Publishers: Utility of Noninvasive Serum Biomarkers of Liver F...
Juniper Publishers: Utility of Noninvasive Serum Biomarkers of Liver F...: ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS Authored by Mostafa M Sira Abstract Background:...
Juniper Publishers: Is Telomere Shortening a Genetic Factor That Predi...
Juniper Publishers: Is Telomere Shortening a Genetic Factor That Predi...: CURRENT RESEARCH IN DIABETES & OBESITY JOURNAL JUNIPER PUBLISHERS Authored by Murillo Ortiz Blanca Abstract Telom...
Juniper Publishers: Oocyte Quality and Female Infertilitye_Juniper Pub...
Juniper Publishers: Oocyte Quality and Female Infertilitye_Juniper Pub...: GLOBAL JOURNAL OF REPRODUCTIVE MEDICINE - JUNIPER PUBLISHERS Authored by Chaube SK Abstract Female infertility is one...
Juniper Publishers: Managing Water Resources Using - Water Radioactive...
Juniper Publishers: Managing Water Resources Using - Water Radioactive...: Agricultural Research & Technology: Open Access Journal - Juniper Publishers Opinion Radioactive contamination, also called rad...
Friday, 20 September 2019
Juniper Publishers: Utility of Noninvasive Serum Biomarkers of Liver F...
Juniper Publishers: Utility of Noninvasive Serum Biomarkers of Liver F...: ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS Authored by Mostafa M Sira Abstract Background:...
Juniper Publishers: Oocyte Quality and Female Infertilitye_Juniper Pub...
Juniper Publishers: Oocyte Quality and Female Infertilitye_Juniper Pub...: GLOBAL JOURNAL OF REPRODUCTIVE MEDICINE - JUNIPER PUBLISHERS Authored by Chaube SK Abstract Female infertility is one...
Thursday, 19 September 2019
Epidemiologic and Clinical Features of Uveitis from a Tertiary Referral Hospital in Bulgaria from 2016-Juniper Publishers
JUNIPER
PUBLISHERS- JOJ Ophthalmology
Abstract
Purpose: The aim of the present study is to
describe the epidemiological and clinical features of recently presented
patients with uveitis in a tertiary referral hospital in Bulgaria.
Material and methods: We conducted a
retrospective observational study on the clinical records of 42 patients
with uveitis of the Department of Ophthalmology, Alexandrovska Eye
Hospital, Medical University - Sofia, Bulgaria. The period of the study
was from March 2016 until December 2016. Follow-up ranged from 1 to 9
months. The diagnosis of the individual cases was based on a complete
eye examination, review of systems, and additional laboratory and
specialized testing methods.
Results: Forty-two new patients with uveitis
presented to our clinic in 2016. Out of them, 28 (66.7%) were female and
14 (33.3%) - male (2:1 ratio). With the exception of one, who was
racially mongoloid, all cases were white-caucasian. The age of the
patients varied from 28 to 70 years, with a mean value of 51.9, median -
50.5, and mode of 40 years. Uveitis was bilateral in 25 (59.5%) and
monolateral in 17 (40.5%) cases. We observed 17 cases (40.5%) of
anterior uveitis, 5 patients (11.9%) with posterior, and 20 (47.6%) with
panuveitis. The major infectious etiologic agents were viruses from the
herpes family, namely herpes simplex virus type -1 and varciella-zoster
virus and toxoplasma gondii.
Conclusion: Uveitis comprises a diverse group
of inflammatory conditions, which affect people of both genders and all
ethnic groups at a relatively young and active age. Visual and anatomic
outcomes may be excellent with timely diagnosis and treatment to prevent
the development of vision-threatening complications. The epidemiologic
data from this small cohort of patients from Bulgaria corresponds well
with the already published literature for other different ethnic groups.
The most common infectious etiologic agents for anterior and panuveitis
belonged to the herpetic viruses family - 16.7%. Non-infectious uveitis
was associated most often with seronegative spondyloarthropathies and
sarcoidosis.47.6% of all cases were classified as idiopathic.
Keywords: Uveitis; Epidemiology; PanuveitisIntroduction
Uveitis is a broad concept, defining inflammation of
the uveal tract, consisting of the iris, ciliary body, and choroid. Any
compartment of the uvea may be affected distinctly or in association
with the other parts and/or additional ocular structures [1,2]. Epidemiologically uveitis has been described in people of both genders, all ages, and in every racial group [1-3].
However, data regarding uveitis cases from Bulgaria, Europe, are
lacking. The etiology is extremely diverse and there are many infectious
and noninfectios conditions which may incite intraocular inflammation [1,2].
The presence of intraocular inflammation may lead to serious and
irreversible vision-threatening structural and functional complications [1,2,4].
Purpose
The aim of the present study is to describe the
epidemiological and clinical features of recently presented patients
with uveitis in a tertiary referral centre in Bulgaria.
Material and Methods
We conducted a retrospective observational study on
the clinical records of 42 patients with uveitis of the Department of
Ophthalmology, Alexandrovska Eye Hospital, Medical University - Sofia,
Bulgaria. The period of the study was from March 2016 until December
2016. Follow-up ranged from 1 to 9 months. All uveitis patients who had
presented prior to March 2016 were excluded from the study. The research
was done with the consent and agreement of the Head of the Department
of Ophthalmology. The diagnosis of the individual cases was based on a
complete eye examination, review of systems, and additional laboratory
and specialized testing methods. For data analysis, descriptive
statistical methods were used.
Results
Forty-two new patients with uveitis presented to our
clinic in 2016. Out of them, 28 (66.7%) were female and 14 (33.3%) -
male (2:1 ratio). With the exception of one, who was racially mongoloid,
all cases were white-caucasian. The age of the patients varied from 28
to 70 years, with a mean value of 51.9, median - 50.5, and mode of 40
years. Uveitis was bilateral in 25 (59.5%) and monolateral in 17 (40.5%)
cases. From anatomical standpoint, we distinguished 17 cases (40.5%) of
anterior uveitis, 5 patients (11.9%) with posterior, and 20 (47.6%)
with panuveitis. No cases of distinct intermediate uveitis were observed
in this cohort.
With regard to anterior uveitis, there were 11
female(64.7%) and 6 male patients (35.3%). Bilateral involvement was
noted in 8 cases (47.1%) and monocular in 9 (52.9%). The presenting age
was from 30 to 78, and most often 40 years (mean 55.9, median 58, mode
40). The inflammation was acute in 8 (47.1%) patients (monocular
involvement in all but one), recurrent - in 4 (23.5%), and chronic in - 5
(29.4%), most often bilateral. Etiologically, it was associated with
herpetic infection in 3 (17.6%) cases (keratouveitis), toxoplasmosis
(manifesting as Fuchs heterochromic phenotype) - 1 (5.9%), psoriasis -
in 2 (11.8%) (one with scleral involvement), Bechterew spondyloarthritis
- in 1 (5.9%), reactive arthritis - in 1 (5.9%), cataract surgery - 1
(5.9%), corneal trauma with vegetable matter - in 1 (5.9%), antiglaucoma
medications (dorzolamide/ timolol and brimonidine) -1, and no definite
extraocular cause was assumed in 6 (35.3%). The visual acuity ranged
between no light perception and 20/20, most frequently - 20/20. The
ocular complications observed were most commonly ocular hypertension in 4
patients (23.5%), cataract - in 3 (17.6%), macular oedema - in 2
(11.8%), posterior synechiae- in 2 (11.8%), corneal scarring - in 1
(5.9%).
Concerning posterior uveitis, there were 3 female
(60%) and 2 male (40%) patients. Bilateral involvement was noted in 3
cases (60%) and monocular in 2 (40%). The presenting age was from 28 to
50 (mean 39, median 40, mode - not applicable). The inflammation was
chronic in 4 patients (80%) and recurrent - in 1 (20%). Etiologically
all cases were idiopathic. Two male patients conformed to the punctate
inner choroiditis (PIC) type of uveitis and one of them had Bechterew
spondyloarthritis. One woman had focal granulomatous inflammation with
adjacent vasculitis with evidence of old foci of inflammation in the
retinal periphery. There was one case with bilateral serpiginous-like
chorioretinitis with associated retinal optic nerve arteriolitis and one
female with uveitis resembling either PIC or acute posterior multifocal
pigment epitheliitis. Visual acuity varied from counting fingers to
20/20, most commonly - 20/25. The major disturbing complaint was
metamorhopsia. The ocular complications were most commonly intraretinal
hemorrhages in 2 cases (40%), atrophy of the retinal pigment epithelium
and outer retinal layers- in 4 eyes (80%), choroidal neovascular
membrane and macular oedema - in 1 eye (20%). From the associated ocular
conditions, 4 patients (80%) had myopia.
Panuveitis was encountered slightly more frequently
than the other types, mostly because of our tertiary referral centre
status. There were 14 female (70%) and 6 male (30%) patients. Bilateral
involvement was noted in 14 (70%) and monocular in 6 (30%) of the cases.
The presenting age was from 30 to 76 - mean 51.7 years. The
inflammation was acute in 1 (5%), recurrent - 8 (40%), and chronic in 11
cases (55%). Final visual acuity ranged between no light perception and
20/20, on average 20/50. Etiologically we found associations with
herpetic infection in 4 patients (20%), sarcoidosis - in 4 (20%),
toxoplasmosis in -1 (5%), Behcet disease - in 1 (5%), malignant
hypertension (masquerade syndrome) - in 1 (5%), and the remaining 9
(45%) were designated as idiopathic. The ocular complications included -
cataract - in 7 patients (35%), preretinal membrane - in 6 (30%),
ocular hypertension - in 5 (25%), macular oedema - in 4 (20%), secondary
glaucoma - in 3 (15%), retinal detachment - in 3 (15%), vireopapillary
traction syndrome - in 3 (15%), posterior synechiae - in 3 (15%),
extensive chorioretinal atrophy - in 2 (10%), anterior synechiae - in 1
(5%), optic nerve atrophy - in 1 (5%), vitreoretinal traction syndrome -
in 1 (5%), hypotony - in 1 (5%).
Discussion
In general, uveitis was not a common diagnosis at our
institution for a period of 9 months. In terms of gender and age, our
data correspond to the already published figures, indication overall
female preponderance [1,5,6] and onset most frequently around the age of 40 [1,2,7,8].
This was especially true for the cases of anterior and panuveitis,
regardless of the diverse etiology. Anterior uveitis is usually the most
common type of intraocular inflammation reported worldwide [1,2].
In the present study, however, panuveitis was the most frequent uveitis
entity at 47.6%, but we assume this to be due to referral bias.
Concerning the causative factors the major infectious
agents were viruses from the herpes family, namely Herpes simplex virus
type -1 and Varciella-zoster virus, and toxoplasma gondii. In those
cases the diagnosis was corroborated by typical clinical findings,
polymerase chain reaction of aqueous humour, and the response to
therapy. With regard to noninfectious causes of uveitis, seronegative
spondyloarthropathies were associated with 4 cases of anterior uveitis,
sarcoidosis - with 4 patients with panuveitis, and Behcet disease with 1
patient with bilateral generalized intraocular inflammation. Secondary
to failure to identify definitive etiologic factors, many cases were
classified as being idiopathic - 6 with anterior uveitis (35%), all 5
with posterior (100%), and 9 with panuveitis (45%). All in all, 20 cases
were idiopathic (47.6%). There was a relatively high frequence of
myopia in the patients with posterior uveitis in our group, which had
also been described for similar cases by other authors [1].
The visual prognosis was excellent in the cohort with
anterior uveitis and it was twice as worse and guarded in those with
panuveitis. Timely and sensible treatment were the necessary conditions
for a good outcome. The reason for the poorer vision in the panuveitis
group was largelly due to a significant delay in the institution of
systemic therapy, including immunomodulatory medications, which had led
to the development of irreversible vision-limiting complications.
The ocular complications of uveitis were not
infrequent and often there were multiple alterations in a single
patient. Structural and functional complications were observed more
frequently in the panuveitis group and in the whole cohort consisted
predominantly of cataract (23.8%), ocular hypertension (21.4%), macular
oedema (16.7%), and preretinal membrane (14.3%). Some of those would
necessitate additional conservative and surgical treatment. Albeit the
small size of the analyzed sample, the relative percentages of the
various complications are very similar to the reported in the literature
for other populations [1,4,7-11].
Conclusion
Uveitis comprises a diverse group of inflammatory
conditions, which affect people of both genders and all ethnic groups at
a relatively young and active age. Visual and anatomic outcomes may be
excellent with timely diagnosis and treatment to prevent the development
of vision-threatening complications. The epidemiologic data from this
small cohort of patients from Bulgaria corresponds well with the already
published literature for other different ethnic groups. The most common
infectious etiologic agents for anterior and panuveitis belonged to the
herpetic viruses family - 16.7%. Non-infectious uveitis was associated
most often with seronegative spondyloarthropathies and sarcoidosis.
47.6% of all cases were classified as idiopathic.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
Juniper Publishers: Is Telomere Shortening a Genetic Factor That Predi...
Juniper Publishers: Is Telomere Shortening a Genetic Factor That Predi...: CURRENT RESEARCH IN DIABETES & OBESITY JOURNAL JUNIPER PUBLISHERS Authored by Murillo Ortiz Blanca Abstract Telom...
Juniper Publishers: Utility of Noninvasive Serum Biomarkers of Liver F...
Juniper Publishers: Utility of Noninvasive Serum Biomarkers of Liver F...: ADVANCED RESEARCH IN GASTROENTEROLOGY & HEPATOLOGY JUNIPER PUBLISHERS Authored by Mostafa M Sira Abstract Background:...
Wednesday, 18 September 2019
Corneal Perforation after Uneventful Cataract Surgery Associated with Sjögren’s Syndrome-Juniper Publishers
JUNIPER
PUBLISHERS- JOJ Ophthalmology
Case Report
A 77 year old female approached our clinic due to a
progressive visual acuity deterioration lasting several years. She has
been diagnosed with primary Sjögren’s Syndrome for the last 5 years,
with keratoconjunctivitis sicca, Xerostomia and arthritis. Other medical
history included ischemic heart disease and hypertension. Her regular
medications included Amlodipine, Tritace, Cadex, Cardiloc, Plaquenil 400
mg and artificial eye lubricants (saline tears x6/d and Viscotears®
Liquid Gel x1/d). She denied use of punctal plugs or topical
cyclosporine use. On her initial examination best corrected visual
acuity was 6/30 in the right eye and 6/20 in the left eye. Slit lamp
examination showed diffuse superficial punctate ephithelial erosions
(SPK). Intraocular pressure (IOP) was 10 in both eyes. The lens had
nuclear sclerosis and anterior capsular opacity. The retina showed
peripapillary atrophy with mild retinal pigmented epithelium changes. On
April 2015 she underwent uncomplicated right eye cataract
phacoemulsification with posterior chamber intra-ocular lens (IOL)
insertion. First day post operative exam showed no change in visual
acuity, cornea with diffuse SPKs, mild descemet membrane folds with +1
cells in the anterior chamber (AC). Postoperative treatment was topical
Diclofenac (a local NSAID) and Maxitrol (Neomycin sulphate, polymyxin B
sulphate and dexamethazone) drops, 4 times a day each. Artificial tear
drops were continued.

Seven days post operatively, examination revealed
that visual acuity remained 6/60 PH 6/30. The cornea had diffuse dense
SPKs with epithelial edema and a small bulla appeared on the lower half.
The patient was asked to gradually lower the medical treatment dosage.
At the next routinely scheduled postoperative examination
(post-operative day 30), a large inferior para-central corneal erosion
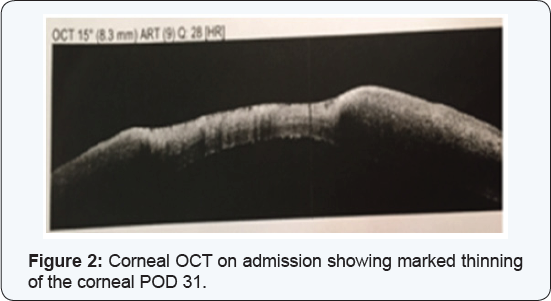
was observed (Figure 1) and corneal OCT showed a significant thinning in the erosion area (Figure2).
The patient reported no pain and didn’t notice any vision
deterioration. On further history, the patient misunderstood her medical
regime and continued both steroidal and NSAIDs drops without lowering
the dosage. She was admitted for hospitalization.
On admission exam visual acuity was 1 meter finger
count (FC), the erosion size was 4.5 mm X 4.2 mm, no infiltrate was
seen, the AC was clear without cells or flare and the PC-IOL was in
place. Serum 20% drops every hour, Erythromycin ointment 4 times a day
and oral Doxycycline 100 mg per day were administered. Maxitrol and
Diclofenac were discontinued. PCR for Herpes Simplex and bacterial
cultures were performed with a negative result. On the second day of
admission visual acuity deteriorated to hand motion. Slit lamp
examination demonstrated a slightly inferior paracentral corneal
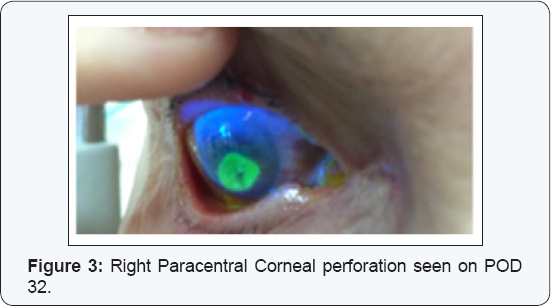
perforation (Figure 3). The AC was shallow and the iris prolapsed through the corneal perforation.
The cornea was glued with cyanoacrylate and a
therapeutic contact lens was placed. Considering corneal melting due to
an inflammatory systemic disease systemic Prednisone 60 mg per day was
initiated. During clinic follow-up the glue remained on the cornea for
about 10 months and a therapeutic contact lens was replaced several
times. After 10 months the glue fell off, at first with a positive
Seidel test but at the concurrent visit there was no more leakage. The
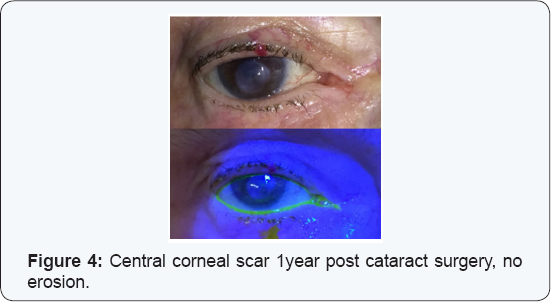
cornea remained with a central corneal scar with no erosion (Figure 4)
and visual acuity did not improve. The patient and her family were not
interested in performing rehabilitative corneal procedures, due to her
system illness.
Discussion
Sjögren’s Syndrome is a progressive autoimmune
disease characterized by lymphocyte infiltration of the exocrine glands
resulting in their fibrosis causing keratoconjunctivitis sicca (dry
eyes; 85% of patients) and xerostomia (dry mouth; 90% of patients) with
several systemic manifestations, [1].
The disease affects mostly women (9:1 ratio) with median age of 54
years. Positive serum serology for Anti SSA (RO) or Anti SSB (LA) is
found in about 60% of patients. The current diagnostic criteria for
Sjögren’s syndrome include ocular or oral symptoms and 2 out of 3 the
following: Positive serum serology (antiSSA and/or antiSSB or positive
rheumatoid factor and antinuclear antibody titer >1:320), salivary
gland biopsy showing tipical lymphocytic sialadenitis (with a focus
score >1 focus/4 mm2) and keratoconjunctivitis sicca (ocular staining
score >3) [1] (Table 1).

The disease is slowly progressing, taking about 10 years from onest until the complete clincal expression is demonsterd[2].
From the ophthalmic point of view the most important symptom is
keratoconjunctivitis sicca, secondary to the lack of tears in the eye
tear film, with destruction of the corneal and conjunctival epithelium.
Treatment is mainly sympthomatic with lubrication or nasolacrimal duct
occlusion. Immunomodulatory treatment as local Cyclosporine has also
been suggested in difficult cases. For systemic manifastations,
treatment may incude Hydroxychloroquine, Methotrexate and Prednisone [2].
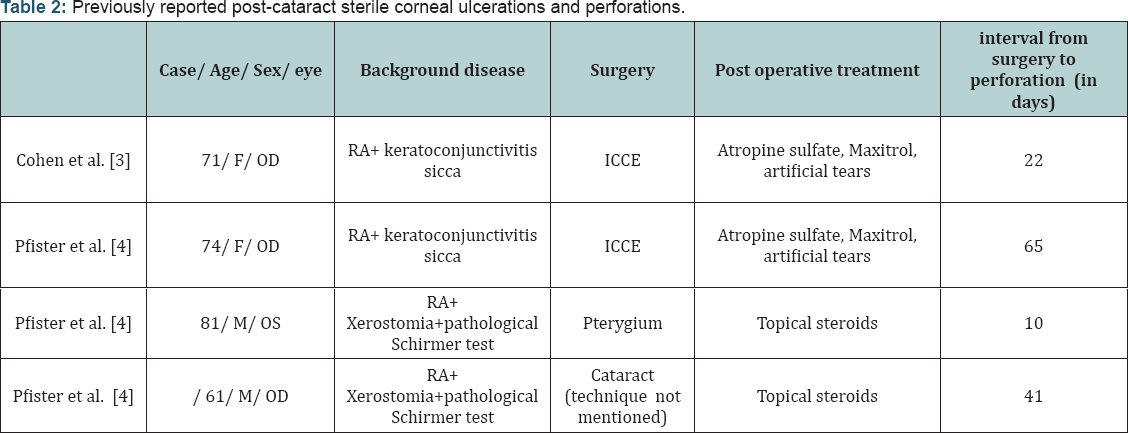
F- Female; ICCE- Intracapsular cataract extraction; RA- Rheumatoid arthritis.
Post-cataract sterile corneal ulcerations and
perforations in Sjögren’s patients has been previously reported in only
two articles, (Table 2) [3,4]. Cohen et al. [3]
reported two females with a prolonged history of rheumatoid arthritis
and keratoconjunctivitis sicca that developed painless sterile corneal
ulceration and perforation following an uneventful cataract surgery
(Intracapsular extraction) [3].
Both patients received postoperative topical steroid drops. As in our
case report, perforations occurred within 3 to 8 weeks following
surgery. Pfister & Murphy [4]
reported on 18 eyes of 14 rheumatoid arthritis and Sjögren’s patients
who had spontaneous corneal ulceration and perforation. Two of the case
occurred following an anterior segment surgery and topical steroid
treatment, one occurred 10 days post Pterygium excision, and the other
cases occurred 42 days post cataract extraction (technique not
mentioned) [4]. Reasons for the perforations in these cases may be divided to:
- A basic anterior segment disease.
- Surgical damage.
- Post-operative injury by topical corticosteroid/ NSAIDS treatment. Strategies for the timely diagnosis and proper management of dry eye syndrome in the face of cataract surgery patients will be emphasized.
A basic anterior segment disease
Patients with Sjögren’s Syndrome may be at a high
risk for complications due to the chronic inflammatory state in the
anterior segment. Sjögren’s Syndrome is characterized by tear film
abnormality and epithelial damage; both are risk factors for
post-operative complications. A study that analyzed corneal innervations
and morphology in primary Sjögren’s Syndrome showed that in comparison
to controls the corneas of Sjögren’s patients had an irregular and
patchy surface epithelium, stromal thinning and that their sub-basal
nerve fiber bundles revealed abnormal morphology [5].
Moreover, in a study following 163 Patients with
Sjögren’s Syndrome, 13% had vision threatening symptoms- 4.5% had
spontaneous corneal melting or perforation during median 3 years follow
up, without any ocular surgery [6].
A chronic ocular inflammation state such as in Sjögren, scleritis or
uveitis patients should be controlled pre-operatively to minimize the
chance of scleral or corneal necrosis. The ophthalmologist can work in
conjunction with other physicians involved in the patient’s care to
consider systemic therapy with systemic corticosteroid and
immunosuppressive agents.
Surgical damage
Anterior segment surgery may cause corneal dryness
and damage by mechanism of post-operative corneal denervation and
reduced blinking rate. During surgery the cornea is exposed for a long
time without blinking which can also contribute to its dryness. Adding
ocular surgery to essentially dry eyes was found as a risk factor for
complications post anterior segment operations [7,8].
Post operative Topical corticosteroid and Non Steroidal treatment
Severe stromal melting has been reported with the
postoperative use of several topical nonsteroidal anti-inflammatory
drugs (NSAIDs). The melting is due in part to the epithelial toxicity
and hypoesthesia that these drugs can induce. In addition topical
steroids suppress corneal wound healing by reducing collagen synthesis [9].
Management of corneal perforation
Persistent epithelial defects accompanied by stromal
lysis require intensive treatment with non-preserved topical lubricants.
The use of topical medications, particularly preserved medications,
should be minimized to reduce epithelial toxicity. Additional treatment
modalities to encourage epithelialization and to arrest stromal melting
include punctal occlusion, bandage contact lenses, tarsorrhaphy,
botulinum injections to induce ptosis, autologous serum eye drops and
systemic tetracycline antibiotics [10].
If the disease continues to progress in spite of medical therapy, an
amniotic membrane graft or lamellar or penetrating keratoplasty should
be considered. Corneal melting may recur even with grafted tissue. For
the treatment of any underlying autoimmune disease, systemic
immunosuppressive therapy may be needed. To note, the prophylactic use
of topical antibiotics must be monitored closely; after a week of
application, many topical antibiotics begin to cause secondary toxic
effects that may inhibit epithelial healing.
Managing patients with high risk for perforation prior to surgery
Abnormalities in the tear film may have an impact on
the ocular surface and thus adversely affect postoperative recovery if
not addressed in advance. Bringing the patient to the optimal epithelial
state prior to surgery will reduce future post-operative complications.
Preoperative excessive lubrications, punctual plugs and even temporal
tarsorrhaphy should be considered[11].
During the surgery itself, we suggest frequent hydration the cornea
with an irrigating solution or by coating the cornea with a topical
viscoelastic agent, in order to reduce such complications. Close
observation of these patients during the weeks following surgery is
warranted to identify and treat toxic keratoconjunctivitis and corneal
ulceration from collagenase activation by postoperative corticosteroid
therapy. Topical NSAID should be used with caution and with close
monitoring for these patients because they have the effect of reducing
corneal sensitivity and thus associated with high risk for corneal
melting [9].
In extreme cases, persistent epithelial defects may require a bandage
(therapeutic) contact lens, tarsorrhaphy, or amniotic membrane
transplant.
Optimizing dry-eye therapy prior to cataract surgery improves visual outcomes [7].
A variety of aqueous layer supportive treatments can be personalized
for each surgical candidate, including topical preserved and
non-preserved liquid tear preparations, gels, and ointments, topical
cyclosporine and punctum plugs. In addition, when planning cataract
surgery, the surgeon must evaluate the patient’s ability to comply with
the postoperative care regimen.
Conclusion
In this report we have discussed the possible factors
for corneal perforation following cataract removal surgery in a patient
suffering from Sjögren’s Syndrome. The effects of severe dry eye may be
potentiated postoperatively due to interference with lid mobility and
corneal denervation, reducing blink rate and post operative treatment
with topical NSAIDS and steroids. We hope to raise surgeon’s awareness
about the importance of proper evaluation of a high risk patient before,
during and after surgery. Meticulously caring for the epithelia may
guarantee good results in high risk patients.
Take home message:
- The effects of severe dry eyes may be potentiated postoperatively due to interference with lid mobility and corneal denervation, reducing blink rate and post operative treatment with topical NSAIDS and steroids.
- It is important to consider close observation of patients with any severity of dry eyes.
- Educate patients about the importance of complying with eye drops and attending follow-up
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
The Use of SWEPT SOURCE OCT ANGIO in Diagnosis and Staging of Type 2 Macular Telangictasia (Mactel 2)-Juniper Publishers
JUNIPER
PUBLISHERS- JOJ Ophthalmology
Abstract
Introduction: Macular
telangiectasia type 2 has also been termed idiopathic perifoveal
telangiectasia or idiopathic juxtafovealtel angiectasis type 2 [1-4]. It
is now referred to as MacTel type 2, and it is a bilateral perifoveal
vasculopathy which originates in the deep retinal capillary plexus in
the temporal juxtafoveal region. As it progresses, it involves the
superficial retinal capillary plexus, and continues to progress
anteriorly, posteriorly, and circumferentially. This is called the
non-proliferative stage of the disease [5-9]. Mactel type 2 becomes
proliferative when the vasogenic process extends under the retina,
forming detachment and a retinal–retinal anastomosis. This form of the
disease may eventually lead to disciform scarring.
Aim & objectives: Diagnosis and staging of macular telangiectasia type 2 (MacTel2) using Swept Source optical coherence tomography Angiography.
Method: We retrospectively
review a 60 Y old patient with bilateral MacTel2 evaluated using a swept
source OCT (SSOCT). The patient underwent a comprehensive ocular
examination and imaging tests as part of the evaluation of her
condition. The imaging tests included color fundus imaging (Topcon,
Tokyo, Japan), digital fundus AF imaging, FA& Swept Source OCT with
OCT Angio (TRITON TOPCON OCT). The patient had no any other retinal
pathology such as diabetic retinopathy or pathologic myopia and not
previously treated with photodynamic therapy (PDT), thermal laser,
intravitreal injections, or any retinal surgery. Information about
previous medical conditions and ocular treatments was obtained by
reviewing the medical charts.
Results: (SS-OCT A) detected
abnormal microvasculature in all MacTel2 eyes, predominantly in the
middle retinal layer. These vessels correlated well with the FA
alterations. The abnormal temporal, juxtafoveal microvasculature in
MacTel2 became apparent as the disease progressed and in later stages
tended to extend circumferentially, with anastomotic vessels temporally.
Conclusion: we used the SS-OCT
Angio technique to investigate eyes with MacTel2 using a TRITON SSOCT.
To extract the blood flow information and visualize the microvasculature
of the central macula, the central macular microvasculature was
visualized better than with FA imaging. In addition, the better
visualization of the juxtafoveal microvasculature with SS-OCT Angio may
also be due, in part, to the absence of leakage on OCT Angio imaging,
and it is this leakage that could obscure the normal vasculature seen on
routine FA imaging. By using this ability to extract and visualize
these retinal layers in MacTel2 and other diseases, SS-OCT Angio imaging
may help facilitate the early diagnosis of disease and provide a better
understanding of disease progression and the efficacy of treatments.
Keywords: Macular telangiectasia Type 2; Swept source oct angiography; Fluorescein angiography; Perifoveal vasculopathyAbbreviations: MacTel 2: Macular Telangiectasia type 2; OCT: Optical Coherence Tomography; SS-OCT Angio: Swept Source OCT Angiography; SD-OCT: Spectral Domain OCT; FA: Fluorescein Angiography; FAF: Fundus Auto Florescence; IS-OS-E: photoreceptor inner segment/outer segment/ellipsoid; GCL+IPL: Ganglion Cell Layer Inner Plexiform Layer; INL + OPL: Inner nuclear layer-Outer Plexiform Layer; ONL + ELM: Outer Nuclear Layer+ External Limiting Membrane; BCVA: Best Corrected Visual Acuity
Introduction
Macular telangiectasia type 2 has also been termed
idiopathic perifoveal telangiectasia or idiopathic juxtafoveal
telangiectasis type 2 [1-3]. It is now referred to as MacTel type 2, and
it is a bilateral perifoveal vasculopathy which originates in the deep
retinal capillary plexus in the temporal juxtafoveal region. As it
progresses, it involves the superficial retinal capillary plexus, and
continues to progress anteriorly, posteriorly, and circumferentially.
This is called the non-proliferative stage of the disease [4-9]. Mactel
type 2 becomes proliferative when the vasogenic process extends under
the retina, forming detachment and a retinal-retinal anastomosis. This
form of the disease may eventually lead to disciform scarring.
In the early stages of the disease, fluorescein angiography
(FA) imaging shows abnormal hyperfluorescence and leakage
from the temporal, juxtafoveal capillary plexus, [7] As the
disease progresses, the hyperfluorescence and leakage
spreads circumferentially around the fovea. While FA provides
a definitive diagnosis of MacTel 2, [10] it also involves the
intravenous injection of a dye that can result in adverse effects
such as nausea or vomiting, and rarely fluorescein can elicit an
anaphylactic response [11,12]. Autofluorescence (AF) imaging
is also useful in diagnosing MacTel2, [13] Due to the depletion
of luteal pigment in the temporal juxtafoveal retina, a relative
increase in AF is observed in this region [14-16]. As the disease
progresses, luteal pigment is lost circumferentially around
the fovea and an increase in the relative hyperfluorescence is
observed. In the later stages of the disease, atrophy of the RPE is
observed, resulting in decreased AF within the central macula.
Optical coherence tomography (OCT), [17] a noninvasive
imaging modality, has revealed structural abnormalities in the
inner retina such as retinal cavitation with draping of the internal
limiting membrane and abnormalities in the outer retina such as
disruption of the photoreceptor inner segment/outer segment/
ellipsoid (IS/OS/E) region that were not previously appreciated
by FA or AF imaging [18-25]. OCT imaging has improved the
early detection of MacTel 2 by identifying these early subtle
changes in retinal anatomy, and OCT has proven to be useful for
following these alterations in macular anatomy as the disease
progresses to foveal atrophy, the formation of intraretinal
pigment plaques, and subretinal neovascularization. With the
development of spectral-domain OCT (SDOCT) instruments with increased scanning speeds and high-speed swept-source OCT (SSOCT)
instruments, OCT microangiography (OMAG) imaging
has emerged as a noninvasive strategy to visualize the retina
and choroidal microvasculature without the use of an exogenous
intravenous dye injection, [26-38] OMAG is a dynamic strategy
capable of providing a three dimensional reconstruction of the
perfused microvasculature within the retina and choroid and
identifying distinct characteristics of the capillary networks
located within different layers of the retina and choroid (see
“Swept-Source OCT Angiography of the Retinal Vasculature Using
Intensity Differentiation-based Optical Microangiography).
Patient and Method
To evaluate the central macular microvascular network in
patients with maculartelangiectasia type 2 (MacTel2) using
Swept Source optical coherence tomography Angiography.
Patient and Method
We retrospectively review a 60 Y old patient with bilateral
MacTel2 evaluated using a swept source OCT (SSOCT).
The
patient underwent a comprehensive ocular examination and
imaging tests as part of the evaluation of her condition. The
imaging tests included color fundus imaging (Topcon, Tokyo,
Japan), digital fundus AF imaging, FA& Swept Source OCT with
OCT Angio (TRITON TOPCON OCT). The patient had no any other retinal pathology such as diabetic retinopathy or pathologic
myopia and not previously treated with photodynamic therapy
(PDT), thermal laser, intravitreal injections, or any retinal
surgery. Information about previous medical conditions and
ocular treatments was obtained by reviewing the medical charts.
The retina was segmented into three distinct physiological
layers: an inner retinal layer from the ganglion cell layer to the
inner plexiform layer (GCL + IPL), a middle retinal layer from the
inner nuclear layer to the outer plexiform layer (INL + OPL), and
an outer retinal layer from outer nuclear layer to the external
limiting membrane (ONL + ELM layer). The microvasculature
from the superficial capillary plexus in the inner retina is
colored red, the microvasculature from the deep capillary plexus
is colored green, and any microvascular structures with flow in
the outer retina are colored blue.
Results
(SS-OCT A) detected abnormal microvasculature in all
MacTel2 eyes, predominantly in the middle retinal layer. These
vessels correlated well with the FA alterations. The abnormal
temporal, juxtafoveal microvasculature in MacTel2 became
apparent as the disease progressed and in later stages tended to
extend circumferentially, with anastomotic vessels temporally.
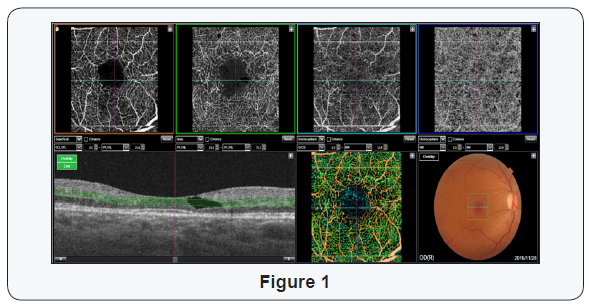
In our Case, the Right Eye was in Early, Non proliferative
MacTel2; best corrected visual acuity (BCVA) in her left eye
was 20/30. The horizontal B scan with the retinal flow in
different layers represented by colors shows the dilated vessels
in the deep retinal capillary plexus found in the middle retinal
layer, most pronounced in the region temporal to the fovea as
observed in green (Figure 1). With intact IS-OS Junction (Figure
2), Fluorescein angiography shows telangiectatic abnormalities
with mild hyperfluorescence and leakage in the temporal
juxtafoveal region (Figure 3).
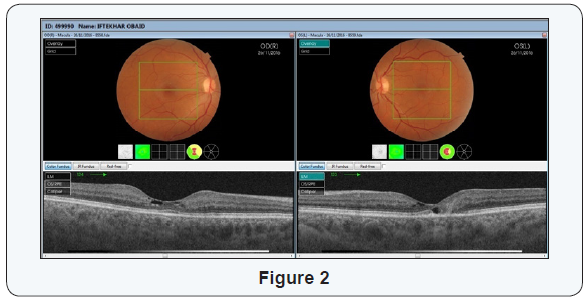


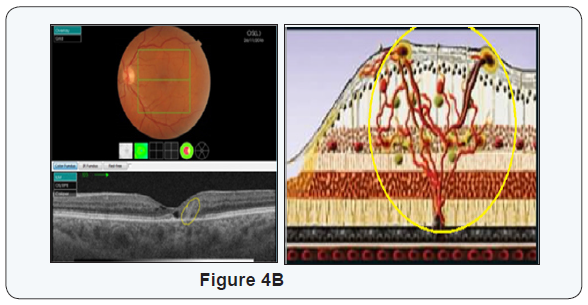
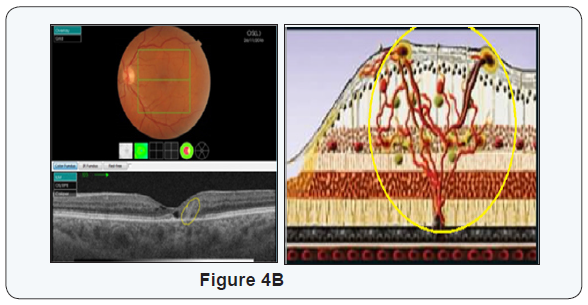
The left eye was in Prolifrative MacTel 2, Best corrected
visual acuity (BCVA) in her left eye was 20/50, The Bscan
shows cavitation in the outer retina and disruption of the IS/
OS/E boundary in the temporal juxtafoveal region. The Bscan
representing the microvascular flow (Figure 4 A&B) details
the presence of abnormal microvasculature (green and blue
corresponding to an area with retinal vascular anastomoses.
Disruption of the microvasculature extends into the outer retina
where the IS/OS/E is disrupted. Microvascular abnormalities,
such as a distorted juxtafoveal capillary plexus with prominent
anastomoses, FA imaging demonstrates hyperfluorescence in
the temporal juxtafoveal region in the earliest stage associated
with late leakage (Figure 5)
Conclusion
We used the SS-OCT Angio technique to investigate eyes
with MacTel2 using a TRITON SSOCT.
To extract the blood flow
information and visualize the microvasculature of the central
macula, the central macular microvasculature was visualized
better than with FA imaging. In addition, the better visualization
of the juxtafoveal microvasculature with SS-OCT Angio may
also be due, in part, to the absence of leakage on OCT Angio
imaging, and it is this leakage that could obscure the normal
vasculature seen on routine FA imaging. By using this ability
to extract and visualize these retinal layers in MacTel2 and
other diseases, SS-OCT Angio imaging may help facilitate the
early diagnosis of disease and provide a better understanding
of disease progression and the efficacy of treatments and to
differentiate MacTel2 from other diseases affecting the retinal
microvasculature associated with fluorescein angiographic
leakage, such as neovascularage-related macular degeneration,
diabetic macular edema, vein occlusions, and cystoid macular
edema from differing conditions.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
Visual Appeal is Important-Juniper Publishers
JUNIPER
PUBLISHERS- JOJ Ophthalmology
Editorial
Fashion and styling have never been more important.
The general trend to want to look beautiful is gathering momentum.
Today, there are more beauty parlours in garages than cars. Newspapers
are full of advertisements luring the bald and greying to regain their
youthful looks with wonder hair oils. Some make tall claims of making
you lose twenty pounds is as many days, with yesterday’s matron
transformed into today’s shapely young thing. And then there are offers
of plastic surgery packages for a nose and face jobs, writes Sabina
Bhatia in a national daily newspaper.
As they say, `first impression is the last
impression’, so good looks play an important role in creating good,
lasting impression. And for good looks you have to have good-fitting and
graciously-looking clothes, well-groomed hair, and a pair of
nice-looking and well-fitting shoes.
For the weak-sighted, today, plenty of good shapes of
spectacle frames are available with a variety of lenses that can truly
enhance the overall personality of an individual. Remember, not wearing
spectacles when required, and in the process straining to see clearly,
is like deliberately and foolishly inviting permanent marks of this
strain on your face.
For those who are simply averse to the use of
spectacles, contact lenses (the invisible aid to vision) in improved
material and disposable variety with single multi-purpose lens-care
solution are available from your eye care practitioner. Following simple
instructions of after-care and contacting one’s eye doctor immediately
in case of need (in the face of an unexpected problem) ensure
comfortable wearing of contacts day-after-day.
And for those who don’t want to go in either for
spectacles or contact lenses, there’s the familiar and proven option of
laser refractive surgery. As a protection from bright sunlight outdoors,
eye-catching designs of sunglasses are available. Expert advice is,
however, helpful in the selection of quality lenses.
For those working on computers and for children who
spend hours together before colour television, UV-protecting glasses are
now available in clear UV-white glass lenses and UV-treated plastic
lenses.
One way of enhancing looks on special occasions like
birthday, marriage-anniversary etc., is to wear cosmetic soft contact
lenses. These come as Plano as well as in power. And the colours are
really bewitching for a natural transition from brown to blue, green,
violet, gray or turquoise or for an altogether different pleasing shade.
Well, visual appeal is now-a-days becoming more and
more important, and as progressive members of the society, we simply
can’t ignore it.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
Tuesday, 17 September 2019
Juniper Publishers: Dynamic Development of Dairy Cow Raising in Vietna...
Juniper Publishers: Dynamic Development of Dairy Cow Raising in Vietna...: Journal of Dairy & Veterinary sciences Juniper Publishers Authored by Hoang Vu Quang, Abstract This paper reviews the deve...
Monday, 16 September 2019
Juniper Publishers: Pilot Study: Pulsed Electromagnetic Field Therapy ...
Juniper Publishers: Pilot Study: Pulsed Electromagnetic Field Therapy ...: Novel Techniques in Arthritis & BoneResearch Juniper Publishers Authored by Magda Havas Abstract This study was designe...
Juniper Publishers: Dynamic Development of Dairy Cow Raising in Vietna...
Juniper Publishers: Dynamic Development of Dairy Cow Raising in Vietna...: Journal of Dairy & Veterinary sciences Juniper Publishers Authored by Hoang Vu Quang, Abstract This paper reviews the deve...
Thursday, 12 September 2019
Visual Appeal is Important-Juniper Publishers
JUNIPER
PUBLISHERS- JOJ Ophthalmology
Editorial
Fashion and styling have never been more important.
The general trend to want to look beautiful is gathering momentum.
Today, there are more beauty parlours in garages than cars. Newspapers
are full of advertisements luring the bald and greying to regain their
youthful looks with wonder hair oils. Some make tall claims of making
you lose twenty pounds is as many days, with yesterday’s matron
transformed into today’s shapely young thing. And then there are offers
of plastic surgery packages for a nose and face jobs, writes Sabina
Bhatia in a national daily newspaper.
As they say, `first impression is the last
impression’, so good looks play an important role in creating good,
lasting impression. And for good looks you have to have good-fitting and
graciously-looking clothes, well-groomed hair, and a pair of
nice-looking and well-fitting shoes.
For the weak-sighted, today, plenty of good shapes of
spectacle frames are available with a variety of lenses that can truly
enhance the overall personality of an individual. Remember, not wearing
spectacles when required, and in the process straining to see clearly,
is like deliberately and foolishly inviting permanent marks of this
strain on your face.
For those who are simply averse to the use of
spectacles, contact lenses (the invisible aid to vision) in improved
material and disposable variety with single multi-purpose lens-care
solution are available from your eye care practitioner. Following simple
instructions of after-care and contacting one’s eye doctor immediately
in case of need (in the face of an unexpected problem) ensure
comfortable wearing of contacts day-after-day.
And for those who don’t want to go in either for
spectacles or contact lenses, there’s the familiar and proven option of
laser refractive surgery. As a protection from bright sunlight outdoors,
eye-catching designs of sunglasses are available. Expert advice is,
however, helpful in the selection of quality lenses.
For those working on computers and for children who
spend hours together before colour television, UV-protecting glasses are
now available in clear UV-white glass lenses and UV-treated plastic
lenses.
One way of enhancing looks on special occasions like
birthday, marriage-anniversary etc., is to wear cosmetic soft contact
lenses. These come as Plano as well as in power. And the colours are
really bewitching for a natural transition from brown to blue, green,
violet, gray or turquoise or for an altogether different pleasing shade.
Well, visual appeal is now-a-days becoming more and
more important, and as progressive members of the society, we simply
can’t ignore it.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
Subscribe to:
Posts (Atom)