JUNIPER
PUBLISHERS- JOJ Ophthalmology
Abstract
Introduction: Macular
telangiectasia type 2 has also been termed idiopathic perifoveal
telangiectasia or idiopathic juxtafovealtel angiectasis type 2 [1-4]. It
is now referred to as MacTel type 2, and it is a bilateral perifoveal
vasculopathy which originates in the deep retinal capillary plexus in
the temporal juxtafoveal region. As it progresses, it involves the
superficial retinal capillary plexus, and continues to progress
anteriorly, posteriorly, and circumferentially. This is called the
non-proliferative stage of the disease [5-9]. Mactel type 2 becomes
proliferative when the vasogenic process extends under the retina,
forming detachment and a retinal–retinal anastomosis. This form of the
disease may eventually lead to disciform scarring.
Aim & objectives: Diagnosis and staging of macular telangiectasia type 2 (MacTel2) using Swept Source optical coherence tomography Angiography.
Method: We retrospectively
review a 60 Y old patient with bilateral MacTel2 evaluated using a swept
source OCT (SSOCT). The patient underwent a comprehensive ocular
examination and imaging tests as part of the evaluation of her
condition. The imaging tests included color fundus imaging (Topcon,
Tokyo, Japan), digital fundus AF imaging, FA& Swept Source OCT with
OCT Angio (TRITON TOPCON OCT). The patient had no any other retinal
pathology such as diabetic retinopathy or pathologic myopia and not
previously treated with photodynamic therapy (PDT), thermal laser,
intravitreal injections, or any retinal surgery. Information about
previous medical conditions and ocular treatments was obtained by
reviewing the medical charts.
Results: (SS-OCT A) detected
abnormal microvasculature in all MacTel2 eyes, predominantly in the
middle retinal layer. These vessels correlated well with the FA
alterations. The abnormal temporal, juxtafoveal microvasculature in
MacTel2 became apparent as the disease progressed and in later stages
tended to extend circumferentially, with anastomotic vessels temporally.
Conclusion: we used the SS-OCT
Angio technique to investigate eyes with MacTel2 using a TRITON SSOCT.
To extract the blood flow information and visualize the microvasculature
of the central macula, the central macular microvasculature was
visualized better than with FA imaging. In addition, the better
visualization of the juxtafoveal microvasculature with SS-OCT Angio may
also be due, in part, to the absence of leakage on OCT Angio imaging,
and it is this leakage that could obscure the normal vasculature seen on
routine FA imaging. By using this ability to extract and visualize
these retinal layers in MacTel2 and other diseases, SS-OCT Angio imaging
may help facilitate the early diagnosis of disease and provide a better
understanding of disease progression and the efficacy of treatments.
Keywords: Macular telangiectasia Type 2; Swept source oct angiography; Fluorescein angiography; Perifoveal vasculopathyAbbreviations: MacTel 2: Macular Telangiectasia type 2; OCT: Optical Coherence Tomography; SS-OCT Angio: Swept Source OCT Angiography; SD-OCT: Spectral Domain OCT; FA: Fluorescein Angiography; FAF: Fundus Auto Florescence; IS-OS-E: photoreceptor inner segment/outer segment/ellipsoid; GCL+IPL: Ganglion Cell Layer Inner Plexiform Layer; INL + OPL: Inner nuclear layer-Outer Plexiform Layer; ONL + ELM: Outer Nuclear Layer+ External Limiting Membrane; BCVA: Best Corrected Visual Acuity
Introduction
Macular telangiectasia type 2 has also been termed
idiopathic perifoveal telangiectasia or idiopathic juxtafoveal
telangiectasis type 2 [1-3]. It is now referred to as MacTel type 2, and
it is a bilateral perifoveal vasculopathy which originates in the deep
retinal capillary plexus in the temporal juxtafoveal region. As it
progresses, it involves the superficial retinal capillary plexus, and
continues to progress anteriorly, posteriorly, and circumferentially.
This is called the non-proliferative stage of the disease [4-9]. Mactel
type 2 becomes proliferative when the vasogenic process extends under
the retina, forming detachment and a retinal-retinal anastomosis. This
form of the disease may eventually lead to disciform scarring.
In the early stages of the disease, fluorescein angiography
(FA) imaging shows abnormal hyperfluorescence and leakage
from the temporal, juxtafoveal capillary plexus, [7] As the
disease progresses, the hyperfluorescence and leakage
spreads circumferentially around the fovea. While FA provides
a definitive diagnosis of MacTel 2, [10] it also involves the
intravenous injection of a dye that can result in adverse effects
such as nausea or vomiting, and rarely fluorescein can elicit an
anaphylactic response [11,12]. Autofluorescence (AF) imaging
is also useful in diagnosing MacTel2, [13] Due to the depletion
of luteal pigment in the temporal juxtafoveal retina, a relative
increase in AF is observed in this region [14-16]. As the disease
progresses, luteal pigment is lost circumferentially around
the fovea and an increase in the relative hyperfluorescence is
observed. In the later stages of the disease, atrophy of the RPE is
observed, resulting in decreased AF within the central macula.
Optical coherence tomography (OCT), [17] a noninvasive
imaging modality, has revealed structural abnormalities in the
inner retina such as retinal cavitation with draping of the internal
limiting membrane and abnormalities in the outer retina such as
disruption of the photoreceptor inner segment/outer segment/
ellipsoid (IS/OS/E) region that were not previously appreciated
by FA or AF imaging [18-25]. OCT imaging has improved the
early detection of MacTel 2 by identifying these early subtle
changes in retinal anatomy, and OCT has proven to be useful for
following these alterations in macular anatomy as the disease
progresses to foveal atrophy, the formation of intraretinal
pigment plaques, and subretinal neovascularization. With the
development of spectral-domain OCT (SDOCT) instruments with increased scanning speeds and high-speed swept-source OCT (SSOCT)
instruments, OCT microangiography (OMAG) imaging
has emerged as a noninvasive strategy to visualize the retina
and choroidal microvasculature without the use of an exogenous
intravenous dye injection, [26-38] OMAG is a dynamic strategy
capable of providing a three dimensional reconstruction of the
perfused microvasculature within the retina and choroid and
identifying distinct characteristics of the capillary networks
located within different layers of the retina and choroid (see
“Swept-Source OCT Angiography of the Retinal Vasculature Using
Intensity Differentiation-based Optical Microangiography).
Patient and Method
To evaluate the central macular microvascular network in
patients with maculartelangiectasia type 2 (MacTel2) using
Swept Source optical coherence tomography Angiography.
Patient and Method
We retrospectively review a 60 Y old patient with bilateral
MacTel2 evaluated using a swept source OCT (SSOCT).
The
patient underwent a comprehensive ocular examination and
imaging tests as part of the evaluation of her condition. The
imaging tests included color fundus imaging (Topcon, Tokyo,
Japan), digital fundus AF imaging, FA& Swept Source OCT with
OCT Angio (TRITON TOPCON OCT). The patient had no any other retinal pathology such as diabetic retinopathy or pathologic
myopia and not previously treated with photodynamic therapy
(PDT), thermal laser, intravitreal injections, or any retinal
surgery. Information about previous medical conditions and
ocular treatments was obtained by reviewing the medical charts.
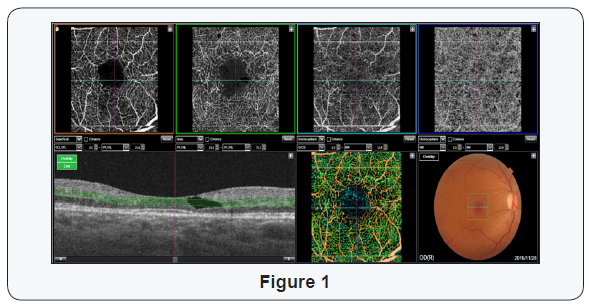
The retina was segmented into three distinct physiological
layers: an inner retinal layer from the ganglion cell layer to the
inner plexiform layer (GCL + IPL), a middle retinal layer from the
inner nuclear layer to the outer plexiform layer (INL + OPL), and
an outer retinal layer from outer nuclear layer to the external
limiting membrane (ONL + ELM layer). The microvasculature
from the superficial capillary plexus in the inner retina is
colored red, the microvasculature from the deep capillary plexus
is colored green, and any microvascular structures with flow in
the outer retina are colored blue.
Results
(SS-OCT A) detected abnormal microvasculature in all
MacTel2 eyes, predominantly in the middle retinal layer. These
vessels correlated well with the FA alterations. The abnormal
temporal, juxtafoveal microvasculature in MacTel2 became
apparent as the disease progressed and in later stages tended to
extend circumferentially, with anastomotic vessels temporally.
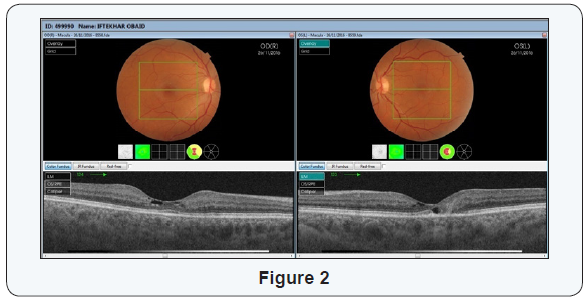
In our Case, the Right Eye was in Early, Non proliferative
MacTel2; best corrected visual acuity (BCVA) in her left eye
was 20/30. The horizontal B scan with the retinal flow in
different layers represented by colors shows the dilated vessels
in the deep retinal capillary plexus found in the middle retinal
layer, most pronounced in the region temporal to the fovea as
observed in green (Figure 1). With intact IS-OS Junction (Figure
2), Fluorescein angiography shows telangiectatic abnormalities
with mild hyperfluorescence and leakage in the temporal
juxtafoveal region (Figure 3).


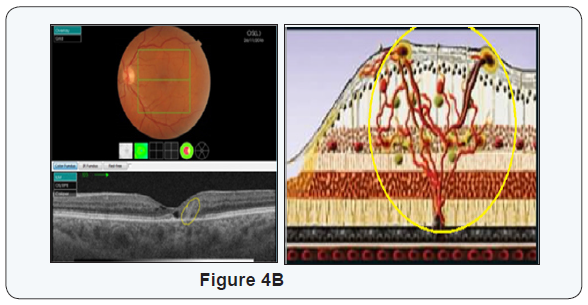
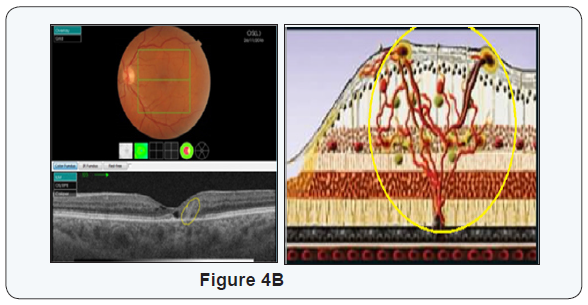
The left eye was in Prolifrative MacTel 2, Best corrected
visual acuity (BCVA) in her left eye was 20/50, The Bscan
shows cavitation in the outer retina and disruption of the IS/
OS/E boundary in the temporal juxtafoveal region. The Bscan
representing the microvascular flow (Figure 4 A&B) details
the presence of abnormal microvasculature (green and blue
corresponding to an area with retinal vascular anastomoses.
Disruption of the microvasculature extends into the outer retina
where the IS/OS/E is disrupted. Microvascular abnormalities,
such as a distorted juxtafoveal capillary plexus with prominent
anastomoses, FA imaging demonstrates hyperfluorescence in
the temporal juxtafoveal region in the earliest stage associated
with late leakage (Figure 5)
Conclusion
We used the SS-OCT Angio technique to investigate eyes
with MacTel2 using a TRITON SSOCT.
To extract the blood flow
information and visualize the microvasculature of the central
macula, the central macular microvasculature was visualized
better than with FA imaging. In addition, the better visualization
of the juxtafoveal microvasculature with SS-OCT Angio may
also be due, in part, to the absence of leakage on OCT Angio
imaging, and it is this leakage that could obscure the normal
vasculature seen on routine FA imaging. By using this ability
to extract and visualize these retinal layers in MacTel2 and
other diseases, SS-OCT Angio imaging may help facilitate the
early diagnosis of disease and provide a better understanding
of disease progression and the efficacy of treatments and to
differentiate MacTel2 from other diseases affecting the retinal
microvasculature associated with fluorescein angiographic
leakage, such as neovascularage-related macular degeneration,
diabetic macular edema, vein occlusions, and cystoid macular
edema from differing conditions.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment