JUNIPER
PUBLISHERS- JOJ Ophthalmology
Case Report
A 77 year old female approached our clinic due to a
progressive visual acuity deterioration lasting several years. She has
been diagnosed with primary Sjögren’s Syndrome for the last 5 years,
with keratoconjunctivitis sicca, Xerostomia and arthritis. Other medical
history included ischemic heart disease and hypertension. Her regular
medications included Amlodipine, Tritace, Cadex, Cardiloc, Plaquenil 400
mg and artificial eye lubricants (saline tears x6/d and Viscotears®
Liquid Gel x1/d). She denied use of punctal plugs or topical
cyclosporine use. On her initial examination best corrected visual
acuity was 6/30 in the right eye and 6/20 in the left eye. Slit lamp
examination showed diffuse superficial punctate ephithelial erosions
(SPK). Intraocular pressure (IOP) was 10 in both eyes. The lens had
nuclear sclerosis and anterior capsular opacity. The retina showed
peripapillary atrophy with mild retinal pigmented epithelium changes. On
April 2015 she underwent uncomplicated right eye cataract
phacoemulsification with posterior chamber intra-ocular lens (IOL)
insertion. First day post operative exam showed no change in visual
acuity, cornea with diffuse SPKs, mild descemet membrane folds with +1
cells in the anterior chamber (AC). Postoperative treatment was topical
Diclofenac (a local NSAID) and Maxitrol (Neomycin sulphate, polymyxin B
sulphate and dexamethazone) drops, 4 times a day each. Artificial tear
drops were continued.

Seven days post operatively, examination revealed
that visual acuity remained 6/60 PH 6/30. The cornea had diffuse dense
SPKs with epithelial edema and a small bulla appeared on the lower half.
The patient was asked to gradually lower the medical treatment dosage.
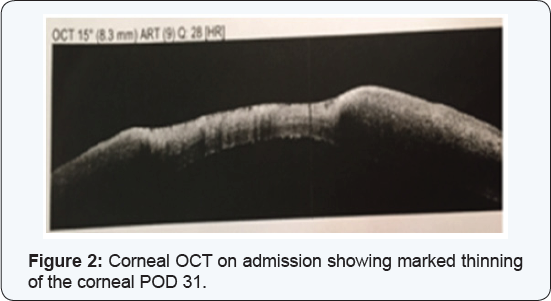
At the next routinely scheduled postoperative examination
(post-operative day 30), a large inferior para-central corneal erosion
was observed (Figure 1) and corneal OCT showed a significant thinning in the erosion area (Figure2).
The patient reported no pain and didn’t notice any vision
deterioration. On further history, the patient misunderstood her medical
regime and continued both steroidal and NSAIDs drops without lowering
the dosage. She was admitted for hospitalization.
On admission exam visual acuity was 1 meter finger
count (FC), the erosion size was 4.5 mm X 4.2 mm, no infiltrate was
seen, the AC was clear without cells or flare and the PC-IOL was in
place. Serum 20% drops every hour, Erythromycin ointment 4 times a day
and oral Doxycycline 100 mg per day were administered. Maxitrol and
Diclofenac were discontinued. PCR for Herpes Simplex and bacterial
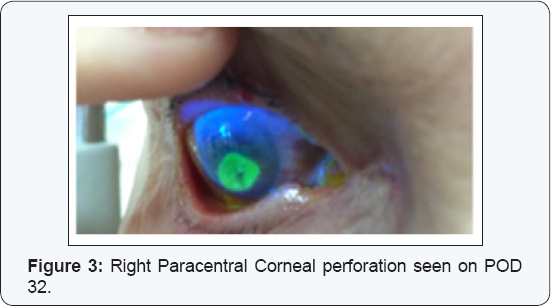
cultures were performed with a negative result. On the second day of
admission visual acuity deteriorated to hand motion. Slit lamp
examination demonstrated a slightly inferior paracentral corneal
perforation (Figure 3). The AC was shallow and the iris prolapsed through the corneal perforation.
The cornea was glued with cyanoacrylate and a
therapeutic contact lens was placed. Considering corneal melting due to
an inflammatory systemic disease systemic Prednisone 60 mg per day was
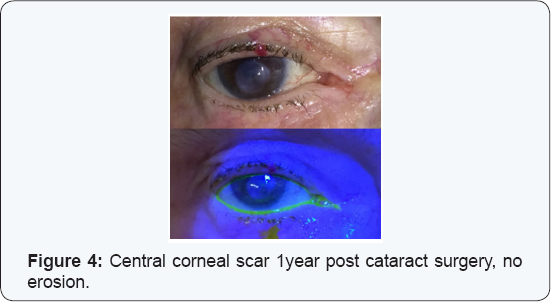
initiated. During clinic follow-up the glue remained on the cornea for
about 10 months and a therapeutic contact lens was replaced several
times. After 10 months the glue fell off, at first with a positive
Seidel test but at the concurrent visit there was no more leakage. The
cornea remained with a central corneal scar with no erosion (Figure 4)
and visual acuity did not improve. The patient and her family were not
interested in performing rehabilitative corneal procedures, due to her
system illness.
Discussion
Sjögren’s Syndrome is a progressive autoimmune
disease characterized by lymphocyte infiltration of the exocrine glands
resulting in their fibrosis causing keratoconjunctivitis sicca (dry
eyes; 85% of patients) and xerostomia (dry mouth; 90% of patients) with
several systemic manifestations, [1].
The disease affects mostly women (9:1 ratio) with median age of 54
years. Positive serum serology for Anti SSA (RO) or Anti SSB (LA) is
found in about 60% of patients. The current diagnostic criteria for
Sjögren’s syndrome include ocular or oral symptoms and 2 out of 3 the
following: Positive serum serology (antiSSA and/or antiSSB or positive
rheumatoid factor and antinuclear antibody titer >1:320), salivary
gland biopsy showing tipical lymphocytic sialadenitis (with a focus
score >1 focus/4 mm2) and keratoconjunctivitis sicca (ocular staining
score >3) [1] (Table 1).

The disease is slowly progressing, taking about 10 years from onest until the complete clincal expression is demonsterd[2].
From the ophthalmic point of view the most important symptom is
keratoconjunctivitis sicca, secondary to the lack of tears in the eye
tear film, with destruction of the corneal and conjunctival epithelium.
Treatment is mainly sympthomatic with lubrication or nasolacrimal duct
occlusion. Immunomodulatory treatment as local Cyclosporine has also
been suggested in difficult cases. For systemic manifastations,
treatment may incude Hydroxychloroquine, Methotrexate and Prednisone [2].
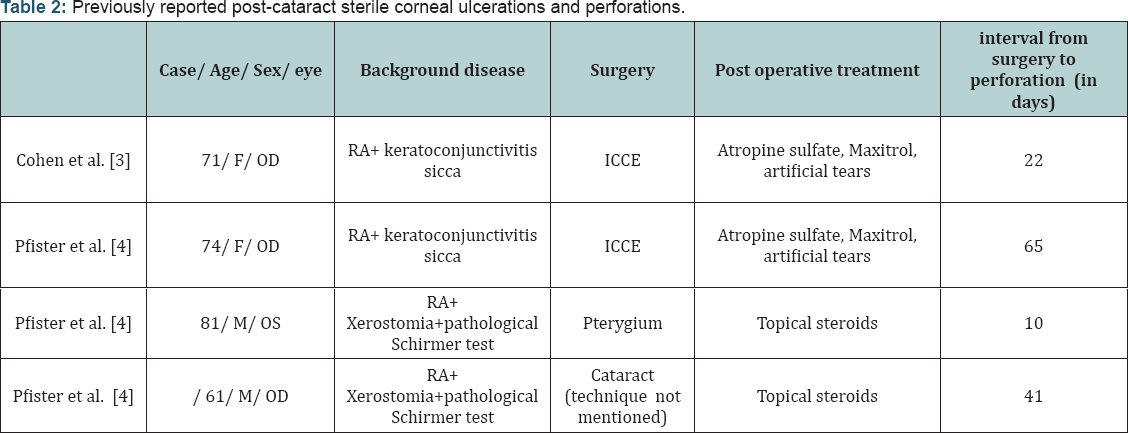
F- Female; ICCE- Intracapsular cataract extraction; RA- Rheumatoid arthritis.
Post-cataract sterile corneal ulcerations and
perforations in Sjögren’s patients has been previously reported in only
two articles, (Table 2) [3,4]. Cohen et al. [3]
reported two females with a prolonged history of rheumatoid arthritis
and keratoconjunctivitis sicca that developed painless sterile corneal
ulceration and perforation following an uneventful cataract surgery
(Intracapsular extraction) [3].
Both patients received postoperative topical steroid drops. As in our
case report, perforations occurred within 3 to 8 weeks following
surgery. Pfister & Murphy [4]
reported on 18 eyes of 14 rheumatoid arthritis and Sjögren’s patients
who had spontaneous corneal ulceration and perforation. Two of the case
occurred following an anterior segment surgery and topical steroid
treatment, one occurred 10 days post Pterygium excision, and the other
cases occurred 42 days post cataract extraction (technique not
mentioned) [4]. Reasons for the perforations in these cases may be divided to:
- A basic anterior segment disease.
- Surgical damage.
- Post-operative injury by topical corticosteroid/ NSAIDS treatment. Strategies for the timely diagnosis and proper management of dry eye syndrome in the face of cataract surgery patients will be emphasized.
A basic anterior segment disease
Patients with Sjögren’s Syndrome may be at a high
risk for complications due to the chronic inflammatory state in the
anterior segment. Sjögren’s Syndrome is characterized by tear film
abnormality and epithelial damage; both are risk factors for
post-operative complications. A study that analyzed corneal innervations
and morphology in primary Sjögren’s Syndrome showed that in comparison
to controls the corneas of Sjögren’s patients had an irregular and
patchy surface epithelium, stromal thinning and that their sub-basal
nerve fiber bundles revealed abnormal morphology [5].
Moreover, in a study following 163 Patients with
Sjögren’s Syndrome, 13% had vision threatening symptoms- 4.5% had
spontaneous corneal melting or perforation during median 3 years follow
up, without any ocular surgery [6].
A chronic ocular inflammation state such as in Sjögren, scleritis or
uveitis patients should be controlled pre-operatively to minimize the
chance of scleral or corneal necrosis. The ophthalmologist can work in
conjunction with other physicians involved in the patient’s care to
consider systemic therapy with systemic corticosteroid and
immunosuppressive agents.
Surgical damage
Anterior segment surgery may cause corneal dryness
and damage by mechanism of post-operative corneal denervation and
reduced blinking rate. During surgery the cornea is exposed for a long
time without blinking which can also contribute to its dryness. Adding
ocular surgery to essentially dry eyes was found as a risk factor for
complications post anterior segment operations [7,8].
Post operative Topical corticosteroid and Non Steroidal treatment
Severe stromal melting has been reported with the
postoperative use of several topical nonsteroidal anti-inflammatory
drugs (NSAIDs). The melting is due in part to the epithelial toxicity
and hypoesthesia that these drugs can induce. In addition topical
steroids suppress corneal wound healing by reducing collagen synthesis [9].
Management of corneal perforation
Persistent epithelial defects accompanied by stromal
lysis require intensive treatment with non-preserved topical lubricants.
The use of topical medications, particularly preserved medications,
should be minimized to reduce epithelial toxicity. Additional treatment
modalities to encourage epithelialization and to arrest stromal melting
include punctal occlusion, bandage contact lenses, tarsorrhaphy,
botulinum injections to induce ptosis, autologous serum eye drops and
systemic tetracycline antibiotics [10].
If the disease continues to progress in spite of medical therapy, an
amniotic membrane graft or lamellar or penetrating keratoplasty should
be considered. Corneal melting may recur even with grafted tissue. For
the treatment of any underlying autoimmune disease, systemic
immunosuppressive therapy may be needed. To note, the prophylactic use
of topical antibiotics must be monitored closely; after a week of
application, many topical antibiotics begin to cause secondary toxic
effects that may inhibit epithelial healing.
Managing patients with high risk for perforation prior to surgery
Abnormalities in the tear film may have an impact on
the ocular surface and thus adversely affect postoperative recovery if
not addressed in advance. Bringing the patient to the optimal epithelial
state prior to surgery will reduce future post-operative complications.
Preoperative excessive lubrications, punctual plugs and even temporal
tarsorrhaphy should be considered[11].
During the surgery itself, we suggest frequent hydration the cornea
with an irrigating solution or by coating the cornea with a topical
viscoelastic agent, in order to reduce such complications. Close
observation of these patients during the weeks following surgery is
warranted to identify and treat toxic keratoconjunctivitis and corneal
ulceration from collagenase activation by postoperative corticosteroid
therapy. Topical NSAID should be used with caution and with close
monitoring for these patients because they have the effect of reducing
corneal sensitivity and thus associated with high risk for corneal
melting [9].
In extreme cases, persistent epithelial defects may require a bandage
(therapeutic) contact lens, tarsorrhaphy, or amniotic membrane
transplant.
Optimizing dry-eye therapy prior to cataract surgery improves visual outcomes [7].
A variety of aqueous layer supportive treatments can be personalized
for each surgical candidate, including topical preserved and
non-preserved liquid tear preparations, gels, and ointments, topical
cyclosporine and punctum plugs. In addition, when planning cataract
surgery, the surgeon must evaluate the patient’s ability to comply with
the postoperative care regimen.
Conclusion
In this report we have discussed the possible factors
for corneal perforation following cataract removal surgery in a patient
suffering from Sjögren’s Syndrome. The effects of severe dry eye may be
potentiated postoperatively due to interference with lid mobility and
corneal denervation, reducing blink rate and post operative treatment
with topical NSAIDS and steroids. We hope to raise surgeon’s awareness
about the importance of proper evaluation of a high risk patient before,
during and after surgery. Meticulously caring for the epithelia may
guarantee good results in high risk patients.
Take home message:
- The effects of severe dry eyes may be potentiated postoperatively due to interference with lid mobility and corneal denervation, reducing blink rate and post operative treatment with topical NSAIDS and steroids.
- It is important to consider close observation of patients with any severity of dry eyes.
- Educate patients about the importance of complying with eye drops and attending follow-up
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment