JUNIPER
PUBLISHERS- JOJ Ophthalmology
Mini Review
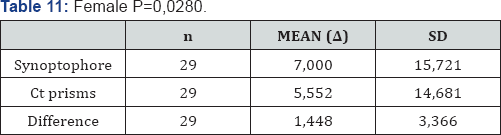
Presenting visual acuity (VA) has been demonstrated
to be the most reliable predictor of the functional outcome in
open globe injuries [1-3]. Eyes with no-light-perception (NLP) post-injury are generally related to poor functional outcomes [4].
Traditionally, primary enucleation had been advocated for severely
traumatized eyes with NLP in view of the risk of sympathetic ophthalmia
[5,6].
Nevertheless, modern immunosuppressives improved the control and
treatment of sympathetic ophthalmia and the reported rates of
sympathetic ophthalmia is as low as 0.3% in recent studies [7].
In addition, NLP at the acute setting does not necessarily mean that
this is irreversible. In the literature, visual recovery rates from NLP
to LP or better vary from 4% to 33% [4,8-11].
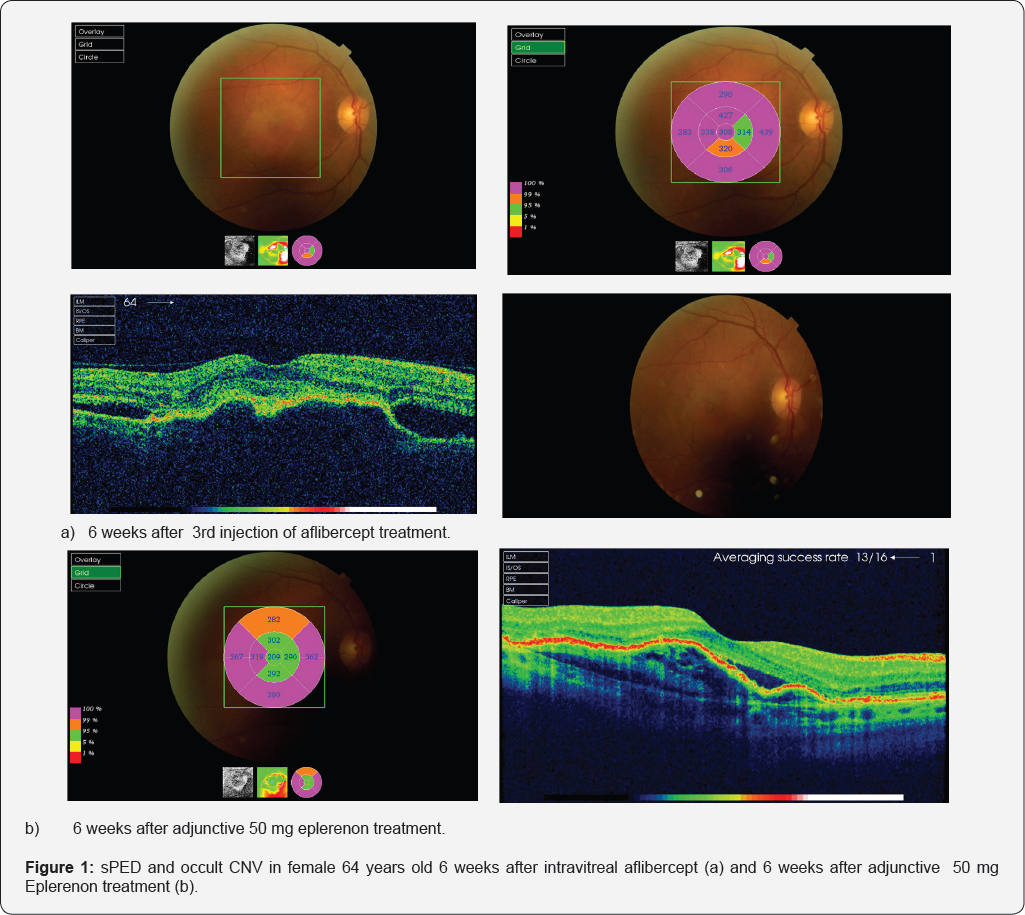
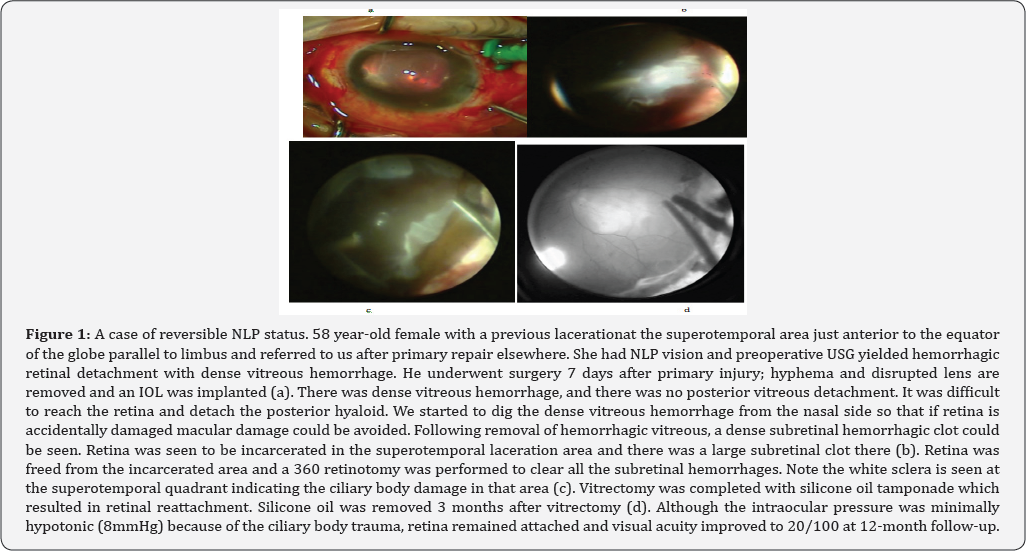
First of all, visual acuity examination in emergency
circumstances is not always reliable because the cognitive status of the
patient (e.g., unconsciousness, anxiety) may easily influence the
result, especially if the examiner is inexperienced. Moreover, most
importantly, visual acuity may be profoundly impaired to the extent of
NLP due to treatable pathologies (e.g., severe corneal edema, hyphema,
dense vitreous and subretinal hemorrhage, particularly in the presence
of retinal detachment, extensive choroidal hemorrhage), correction
of which may reverse NLP status (Figure 1).
Hence, after ascertaining the vision is NLP, clinician must try to
identify if the underlying cause is reversible or irreversible. In eyes
with severe media opacity, B-scan ultrasonography often aids in
diagnosis.
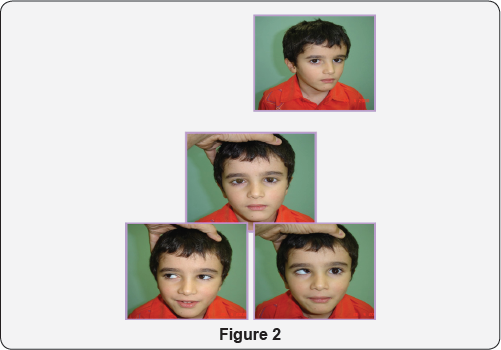
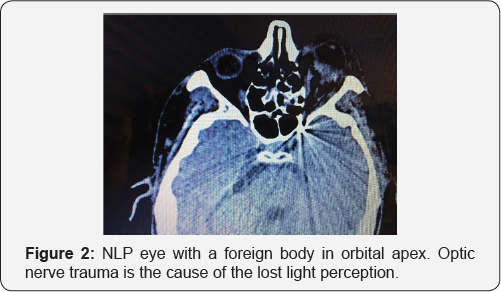
Only in cases of optic nerve transection or complete avulsion, the ophthalmologist may be certain that NLP status is permanent [8,9,12,13] (Figure 2).
Relative afferent pupillary defect (RAPD) is an indicator of optic
nerve damage; however, it may be falsely positive in the presence of
severe hyphema, or subretinal hemorrhage [14].
CT or MRI imaging is successful to demonstrate optic nerve damage
(e.g., avulsion, transection) in most of the cases. Even in these cases
with no visual potential, the aim should be the anatomic salvage of the
globe. Primary enucleation may only be justified if the eye is
deformed to an extent that anatomic closure of the wound is not
possible.
Secondary vitreoretinal surgery has an unquestionably
critical role in preservation of vision and globe. In one study, all
the eyes which had recovered from NLP without having secondary
vitrectomy were observed to become phthisical with NLP vision within 7
months [10].
Another study showed that eyes that underwent secondary vitrectomy
were more likely to recover from NLP vision than those that did not [13].
We advocate early secondary surgery between 3-10 days after open-globe
injury. Performing vitrectomy several days after injury allows media
clarity, wound stabilization and posterior vitreous detachment to set
in. It also has an advantage of decreased uveal congestion which might
otherwise result in uncontrollable hemorrhage [15].
However, deferring vitrectomy more than 2 weeks has severe
disadvantages (proliferative vitreoretinopathy, ciliary body destruction
and consequent phthisis) [16]; hence should be avoided.
Some clinical features may help to predict the visual
prognosis of traumatized eyes with NLP after vitreoretinal surgery.
Bhagat et al. [13]
suggested that NLP eyes that had recovered LP or better vision on the
first postoperative day after primary repair might be more likely to
recover from NLP at the last follow-up compared to the eyes having NLP
on the first postoperative day (71% vs. 8%) [13]. Salehi-Had et al. [10]
showed that eyes which had recovered LP or better vision within 5 days
of primary repair and/or had vitreoretinal surgery within 5 weeks of the
initial injury achieved a more favorable visual outcome [10].
Ciliary body damage, closed funnel retinal detachment, or choroidal
damage, on the other hand, has found to be risk factors for developing
NLP post trauma [12].
Presence of RAPD and zone 3 wound extending beyond rectus insertion
are other clinical features that have been shown to be associated with
poor visual prognosis [8].
However, it should be kept in mind that these clinical findings do not
necessarily indicate a definite NLP status. Awareness of visual
prognosis prior to surgery is important in appropriate management
strategy as well as patient counseling.
Given the low risk of sympathetic ophthalmia and
advances in vitreoretinal surgical techniques, we recommend globe
salvaging procedures for severely traumatized NLP eyes, unless the
anatomic reconstruction is impossible. Appropriate primary repair and
timely vitreoretinal intervention may give a chance for visual recovery.
Even in cases with permanent visual loss, anatomic preservation of
the globe should be the primary purpose as the idea of losing an
eye is a devastating situation to the patient and the family. Secondary
enucleation may be carried out for blind painful cosmetically
unacceptable eyes or at the patient's request.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php