Comparing the Sensitivity of Visual Evoked Potential and Standard Achromatic Perimetry in Diagnosis of Optic Neuritis- Juniper Publishers
Juniper Publishers- JOJ Ophthalmology
Abstract
Purpose: To evaluate the diagnostic power of Visual
Evoked Potential (VEP) and Standard Achromatic Perimetry (SAP) in a
group of patients with Multiple Sclerosis (MS) and a history of optic
neuritis (ON).
Methods: 136 eyes of 68 patients (11 male and 57
female, average age 27.18 years) with a confirmed diagnosis of MS
underwent SAP and pattern VEPs. 67 eyes (49.2%) had no history of ocular
involvement and a negative ophthalmologic examination, while 69 had
proven ON according to physical examination. The mean deviation (MD) and
the pattern standard deviation (PSD) of perimetry and the amplitude
& latency of VEP in both normal and abnormal eyes were recorded. MD
& PSD<0.5% and pl00 latency more than 118 millisecond were
considered abnormal.
Results: MD was abnormal in 93.9% of the eyes with
ON, PSD was abnormal in 69.4% and latency was abnormal in 55% of the
affected eyes with ON. In overall, VEP can diagnose 55% of the eyes
affected with ON and SAP can diagnose 96%. In statistical analysis of
MD, PSD, latency and amplitude values with Mann-Whitney Test MD and PSD
were statistically significant (MD has p<0.001, PSD has P<0.05,
latency has p=0.83 and amplitude has p=0.38).
Conclusion: The results of this study demonstrate
that SAP is more sensitive than VEP in the diagnosis of ON. SAP is a
less operator and patient dependent technique and the patient test
reliability can be assessed with parameters such as False-positive
response rate, False- negative response rate, Fixation loss &
Short-term fluctuation measurement. Because of these advantages, SAP has
better sensitivity than VEP in the diagnosis of ON. Our results suggest
that clinical and subclinical visual involvement of ON can be better
diagnosed using both SAP and VEP tests, together.
Keywords: Keywords: Diagnostic power of SAP & VEP; Multiple sclerosis Introduction
Multiple sclerosis (MS) is an autoimmune disease that
involves the Optic Nerve, brain and spinal cord by damaging the myelin
sheath [1].
The disease can affect patients' visual pathway and therefore lead to
Optic Neuritis (ON) which is an eye discomfort accompanied by decreased
visual acuity, changes in the visual field, uncontrollable rapid eye
movements and double vision (clinical and frequent subclinical evident
manifestations) [1-3]. De-myelinating disease leads to less responses of the brain and the optic nerve which is detected by the visual evoked.
potential [3-5].
Alterations in the visual evoked potential (VEP) and standard
achromatic perimetry (SAP) have been reported to be useful in patients
with MS. Many studies have shown the presence of abnormality in the
results of VEP and SAP in optic neuritis [6], but there is little agreement about the prevalence of these abnormalities or about which examination is more sensitive [7-10].
In this article, our aim is to evaluate the diagnostic power of SAP
& VEP in a group of patients with Multiple Sclerosis (MS) and a
history of optic neuritis.
Material and Methods
Sixty eight patients with ON and MS were recruited
from the neurology and neuro-ophthalmology clinics of Rassoul Akram
hospital in 2010-2011. The diagnosis of ON/MS was made based on standard
clinical symptoms, examination findings, and radiologic abnormalities.
In all patients, the disease was in remission and no patient was
affected by any general disease apart from MS [11].
The diagnosis of ON was based on clinical signs and
symptoms; such as: history of a progressive decrease of vision, color
vision deficit, painful eye movements, fundus examination and relative
afferent pupillary defect (RAPD) which is diagnosed by a neurologist or
neuro-ophthalmologist. Patients voluntarily participated in this study
and all participants were enrolled after an informed consent was
obtained. All patients underwent full ophthalmic examination, including
best-corrected visual acuity (BCVA) measurement, slit lamp
biomicroscopy, applantation tonometry, and fundus examination after
pupillary dilation. VEP pattern reversal was performed (Sirius Galileo;
Esaote Biomedica, Florence, Italy). Latency and amplitude were recorded
and AP100 latency>118ms (i.e., 2SD above the mean) was considered
abnormal.
Standard achromatic perimetry (SAP) was performed by
means ofthe Humphrey Field Analyzer 750 (model 750; Carl Zeiss Meditec,
Dublin, CA) using the 30-2 program with the Swedish interactive
threshold algorithm (SITA) standard strategy. Two consecutive visual
field examinations were performed for each patient, but only the second
was evaluated for the purpose of the study and only if reliability
indices were normal. The criteria for abnormality were mean deviation
(MD) or pattern standard deviation (PSD) and were labeled abnormal by
the instrument's software. VEP and SAP were done for all patients with
one expert optometrist.
Patient data were collected through questionnaires,
respectively, were entered into the SPSS software version 18.0 and were
then analyzed. Maximum, minimum, and SD±Mean were reported for the
quantitative data and for the qualitative data, the number (percentage)
was stated. The Chi-Square test, with the aid of SPPS software was used
to evaluate the relationship between qualitative variables and
Mann-Whitney test was used for evaluation of normality between data and a
P-value of<0.05 was considered valuable. VEP and SAP were done in
all 68 patients (136 eyes). The age, sex, MD, PSD, amplitude and latency
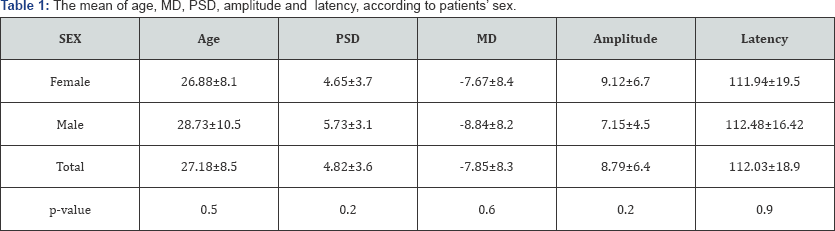
recorded are shown in Table 1.
Results
From the 68 patients that were included in this
study, 11 were male (16.2%) and 57 were female (83.8%). The mean±SD age
of the patients was 27.18±8.5 (range:14-61 years old). 49.6% of the eyes
that were included in the study were normal and 50.4% had ON. The mean
MD value was -7.86db (with SD: 8.4) with a range of -34.49db to7.57db.
Also, the mean±SD MD value in normal eyes was -4.89db±7.12 with a range
of -34.49db and 7.57db, while the mean value±SD of MD in the affected
eyes was-10.63db±8.98 with a minimum of -31.28db and a 5.18db maximum.
MD was negative in 19.1 % of the normal eyes and positive in 80.9%,
while being negative in 6.1% and positive in 93.9% of the eyes affected
with ON. The mean±SD, PSD value was 4.82d3.6 with a minimum of 1.06db
and a maximum of 14.46db. PSD value in normal eyes had a mean±SD of
3.55db±3.09 with a minimum and maximum of 1.06db and 14.13db; and the
mean value of PSD in affected eyes was 5.78db (SD: ±3.75) with a minimum
of 1.34db and a 14.13db maximum. PSD was negative in 59.6% and positive
in 40.4% of the normal eyes and 30.6% negative and 69.4% positive in
the affected eyes with ON.
The mean±SD latency value was 112.03ms±18.98 with a
range of 58ms to 157ms. The mean±SD latency value in normal eyes was
109.98ms±17.03 with a range of 58ms to 157ms while in the affected eyes,
the mean±SD value of latency was 114.07ms±19.85 with a 58ms minimum and
a maximum of 150ms. Also, latency was negative in 70.6% and positive in
29.4% of the normal eyes, while being 45% negative and 55% positive in
the affected eyes with ON.
The mean±SD amplitude value was 8.79μv±6.41 with the
minimum of 0.5μv and a maximum of 34.9μv. The mean±SD amplitude value in
normal eyes was 10.04μv±6.76 with a range of 1.13μv to 27.90μv and in
the affected eyes, the mean±SD value of amplitude was 7.71μv±5.86 with a
0.50μv minimum and a maximum of 27.90μv.
In statistical analysis of MD, PSD, latency and
amplitude P<0.05, that statistically significant but latency has
p=0.83 and values with Mann-Whitney Test, MD has p<0.001, PSD has
amplitude has p=0.38 (Table2).

Discussion
In many studies, subclinical alterations can be
helpful in diagnosing some cases of the visual system in both normal and
Multiple Sclerosis patients, but we found that there was little
agreement about the prevalence of these abnormalities [12-15]
and the fact that which abnormality has the most sensitivity(6,14). In
our study there was no single examination detected in all cases of
visual involvement. So, the VEP P100 latency is the most diffuse and
also the parameter of it had been used for detection the optic nerve
involvement, but it is not very sensitive for the diagnosis of post
chiasmal localizations. The results of our study had been impacted by
other related studies too.
On other hand, the result of other studies shows that the VEP P100 latency cannot detect all cases of optic nerve involvement [10].
Also, some studies demonstrate that automated perimetery can too be an
excellent tool in evaluating neuro-ophthalmologic disorders. Our studies
show that SAP is more sensitive than VEP in the diagnosis of ON. In
overall, VEP can diagnose 55% of the affected eyes with ON and SAP can
diagnose 96%. In statistical analysis of MD, PSD, latency and amplitude
values with Mann- Whitney Test, MD has p<0.001 and PSD has P<0.05
and latency has p=0.83 and amplitude has p=0.38. SAP and is a less
operator and patient-dependent technique and the patient test
reliability can be assessed with parameters such as False-positive
response rate, False-negative response rate, Fixation loss &
Short-term fluctuation measurement.
In an article by Ruseckaite R et al. [16],
the results on Frequency doubling illusion VEPs and automated perimetry
in Multiple Sclerosis is shown. The recordings in the study were
obtained from 27 Normal subjects, 26MS patients who had experienced
Optic Neuritis (MSON) and 24MS patients without a history of ON (MSNON).
Ruseckaite R et al. [16]
study also demonstrated that discriminant models based on the Frequency
Doubling Technology (FDT) thresholds and multi focal VEP (mfVEPs) were
able to diagnose more that 90% of MSON patients, but performed poorly
for MSNON patients.
Because of these advantages, SAP can have better
sensitivity than VEP in the diagnosis of ON. (96%vs55%). Other
advantages of SAP are as follows:
- Standardized testing conditions, which allow better serial and inter- institutional comparisons of fields
- Less technician dependence which improves sensitivity.
- Producing numerical data that are amenable to statistical analysis for comparisons and clinical studies.
In VEP, if a patient loses focus on the target, the
test results may be false negative or false positive. For Most clinical
situations, the VEP is of limited use. It is subject to numerous factors
that may produce abnormal waveforms in the absence of visual pathway
damage, including uncorrected refractive error, media opacity,
amblyopia, fatigue, and inattention (either intentional or
unintentional). In Most cases, the VEP is unnecessary for the diagnosis
of optic neuropathy and is less accurate to quantify it than perimetry [8,9]
The two scenarios in which VEPs remain clinically
useful are: First, the evaluation of the integrity of the visual pathway
in infants or inarticulate adults. In this case, a preserved flash or
pattern response confirms intact pathways and an abnormal flash response
consistently reflects gross impairment. An abnormal pattern response is
less useful, as it may indicate damage or this may be a false- negative
result. Second, confirming intact visual pathways in patients with
markedly abnormal subjective visual responses of a suspected nonorganic
origin [10,11].
Corallo G et al. [17],
in a study about conventional perimetry and visual evoked potentials in
the assessment of patients with Multiple Sclerosis, demonstrated that
the group of asymptomatic subjects had abnormal Conventional Automated
Perimetry (CAP) in 1 eye (6.25%), abnormal Short-wavelength automated
perimetry (SWAP) in 9 (56.2%), abnormal FDT in 11 (68.7%), and abnormal
VEPs in 7 (43.7%). Also, Corallo G et al. [17]
show that the combined use of all techniques allowed the researchers to
identify silent optic nerve impairment in 15 (93.7%) eyes of MS
patients. In another study by Della et al. [18],
on the nerve fiber layer analysis with GDx with a variable corneal
compensator in patients with Multiple Sclerosis, the result is shown
that GDx VCC is less able to detect early defects in MS patients
compared to the currently used standard techniques of SAP and VEPs.
At last in our cases, intact pattern had been
developed a measure of expected acuity when stimuli of various sizes and
confirms an intact visual pathway. Because voluntary inattention or de
focusing may markedly reduce the pattern waveform, again, an abnormal or
absent pattern response does not confirm organic disease.
Conclusion
According to the results of this study and what was
discussed above, we suggest using both VEP and SAP tests for the
diagnosis and follow up of Optic Neuritis in patients with Multiple
Sclerosis.
Declaration
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment