A Comparison of Automated Refractions Using Plusoptix S04 Photoscreener, Nidek AR-20 Handheld Autorefractor and Nidek ARK-510A Auto Ref-Keratometer- Juniper Publishers
Abstract
Purpose: To evaluate automated refraction
measurements using the Plusopti X S04 photo screener (OP), Nidek AR-20
hand held auto refractor (NAR) and compare them to the more traditional
Nidek ARK-510A (ARK).
Methods: 102 patients aged 3 to 81 years were
included. All patients underwent on-cycloplegic automated refraction
using the PlusoptiX S04 photo screener, Nidek AR-20 handheld auto
refractor and the Nidek ARK-510A. This was followed by measuring Cyclo
plegic auto refraction using the Nidek AR-20 handheld auto refractor and
Nidek ARK-510A.
Results: Without Cyclo plegia, the mean sphere
values were significantly different for both the OP (-0.41 D, SD±2.39D)
versus ARK (-0.60D, SD±2.24) groups with a p=0. 008, and for NAR
(-0.48, SD±2.01) Versus ARK groups with a p=0.029. With cycloplegia,
there was no significant difference in the mean sphere values between
the OP versus ARK groups as compared to the OP versus NAR and NAR versus
ARK groups (p=0.049 and p=0.001 respectively).
Conclusion: Our study indicates similarities
between the OP photo screener and the traditional table-mounted ARK
results after cycle plegia. These results were not reflected when
comparing the NAR handheld auto refractor to the ARK. Although efficient
as screening tools, we recommend caution when using handheld
instruments.
Keywords: Refractometer; Refractive errors; Myopia; Hyperopia; Astigmatism; Cycloplegia; Middle east; LebanonIntroduction
Refraction is a clinical test used to determine the
refractive state of the eye and to assess the individual's need for
visual aid. Although hretinoscopy is still considered the gold standard
for determining the refractive state of the eye, it is subject to
interobserver variability [1,2].
Over the past few decades, new advancements have introduced the auto
refractors which have gained a popular routine use among
ophthalmologists [3,4].
Auto refractors are easy to use, time saving and relatively accurate in
measuring the amount and type of refractive error. Today, many auto
refractors are available in the market (Canon, Nikon, Topcon, Carl Zeiss
Meditec, Nidek etc.). A disadvantage of most auto refractors is they
need to be mounted on a table due to their relatively large size. As
such, ametropia measurements may therefore be difficult in bed ridden
patients, disabled persons and very young or handicapped children.
Handheld auto refractors or photo screener scans are useful in such
scenarios.
Plusopti XS04 (OP) (Plusoptix GmbH; Nuremberg,
Germany), is a third generation vision screener designed to screen for
refractive errors, anisocoria, and strabismus in children starting at
the age of 6 months [5].
Screening is quick with both eyes screened simultaneously and can be
performed by non-medical personnel, with a screening distance of 1 meter
[5].
The device measures refraction, pupil size, and corneal reflexes.
Results with abnormal limits are displayed as "refer". Referral criteria
include anisometropia, astigmatism, hyperopia, myopia, anisocoria and
corneal reflexes [5].
To date, multiple studies show that the OP vision
screener is useful when used in screening for amblyopia oramblyogenic
risk factors [6-10] small-angle strabismus [11] is considered effective when compared to cycloplegic pediatric ophthalmic evaluation [9,10]
and can be used to screen patients with intellectual disability
foramblyogenic risk factors with 95% sensitivity and 50% specificity [12].
In our manuscript, we explore the accuracy of both
the OP vision screener when used as suggested in noncyclopleged
patients, the Nidek AR-20 (NAR) (NidekCo. Ltd, Gammagori; Aichi, Japan)
handheld auto refractor on non cyclopleged and cyclopleged patients and
compare the results with those obtained before and after cycloplegia
using a more traditional table- mounted NidekARK-510A (ARK)
autorefractor/keratometer (NidekCo. Ltd, Gammagori, Aichi, Japan).
Materials and Methods
We prospectively evaluated 102 consecutive patients
presenting to the outpatient clinic during August 2013, without any bias
to their age, gender, diagnosis or previous medical history. Patients
were excluded if they could not be refracted because of poor cooperation
or any ocular pathology. After the initial history was taken, a trained
ophthalmology fellow (H.B) and professional optometrist (J.H) used all 3
instruments to obtain non Cyclo plegic automated refraction. This was
followed bycycloplegia using 1 drop of Mydriacyl (tropicamide 1%, Alcon,
Puurs, Belgium) in each eye twice (10 minute interval). Twenty to 30
minutes later, Cyclo plegic auto refraction was obtained using the ARK,
and NAR auto refractors.
Data entry and statistical analysis were performed
using SPSS 22.0 for Windows (SPSS Inc, Chicago, IL, USA). Analysis
variables included:gender, age (years), auto refraction (sphere,
cylinder, axis) and spherical equivalent for both eyes. For each of the
3instruments, the data were divided into 4 main categories: sphere,
cylinder, axis and spherical equivalent. Spherical equivalent (sphere
power+(0.5 x cylinder power)) measured in diopters was calculated from
the auto refraction measurements. For the ARK and NAR handheld auto
refractor, data were further divided into non cycloplegic and Cyclo
plegic auto refractiCases with missing variables were excluded from the
analysis. Two types of statistical testing were used to determine
differences or similarities between the OP, NAR handheld auto refractor,
and the ARK. Analysis of variance (ANOVA) testing was performed to
compare the 3 groups. A variable ratio (F) was calculated to determine
overall statistical differences. Paired-samples t-tests were performed
to compare means between 2 groups. Significance was defined as p values
less than or equal to 0.05.
Results
One hundred two patients (204 eyes) were initially
recruited. Nineteen eyes (9.3%) could not be refracted by OP (one
patient could not be refracted for both eyes by neither OP nor the NAR)
and were excluded from the analysis. A total of 185 eyes completed the
study on all 3 instruments and were included in the analysis (45.7%
males, 54.3% females). The patients ranged in age from 3 years to 81
years (mean 41.02±19.7years, median 43 years).Using OP, the mean
recorded sphere on 185 eyes was -0.41 diopters, mean cylinder was +1
diopters, and mean axis were measured at 90.6° (Table 1).
The median spherical value was Plano (range -6.75 to +10). The mean
spherical equivalent determination of the OP group was +0.09 diopters
(range -6.125 to +10.5). A myopic spherical value was found in 47.6% of
the eyes 42.7%were hyperopic and 9.7% were plano. Astigmatism was
identified in 96.8%
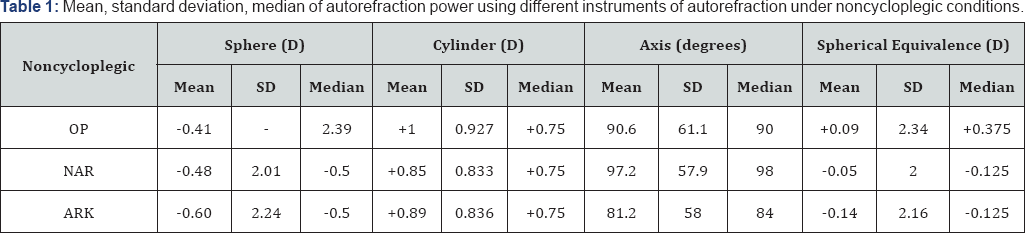
OP:PlusoptiX S04 (Plusoptix GmbH;
Nuremberg, Germany); NAR: Nidek AR-20 (Nidek Co.Ltd, Gammagori; Aichi,
Japan); ARK: Nidek ARK-510A (NidekCo.Ltd, Gammagori; Aichi, Japan).
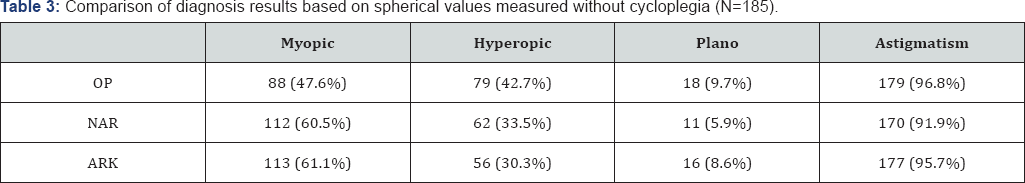
Non cycloplegic auto refraction results for nidek AR-20 handheld autorefractor and nidek ARK-510A
The mean sphere value recorded by the NAR for 185
eyes was -0.48 diopters, mean cylinder was+0.85 diopters, and mean axis
were 97.16°. The median spherical value was -0.5 diopters (range -6.75
to+8.5). The mean spherical equivalence for the NAR group -0.05 diopters
(range -6.125 to+9.12). A myopic spherical value was identified in
60.5%; 33.5% were hyperopic, and 5.9% were Plano. Astigmatism was
identified in 91.9% (Table 3).
The mean spherical value recorded using the ARK on 185 eyes was -0.604
diopters, mean cylinder was +0.89 diopters, and mean axis measurement
was 81.2° (Table 1).
The median spherical value was -0.5 diopters (range -6.25 to+10.5). The
mean spherical equivalence measured in this group was -0.136 diopters
(range -4.875 to+1G.875). A myopic spherical value was diagnosed in
61.1%, 3G.3% were hyperopic, and 8.6% were Plano. Astigmatism was
identified in 95.7% of 185 eyes (Table 3).
Cycloplegicautorefraction results for nidek AR-20 handheld autorefractor and nidek ARK-510A
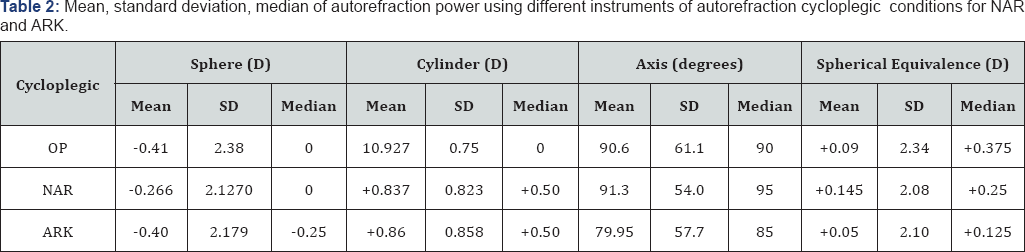
The mean sphere value recorded by the NAR for 185
eyes was -0.266 diopters, mean cylinder was +0.837 diopters, and mean
axis were 91.3° (Table 2).
The median spherical value was Plano (range -5.75 to+10.5). The mean
spherical equivalence for the NAR group +0.145 diopters (range -4.75
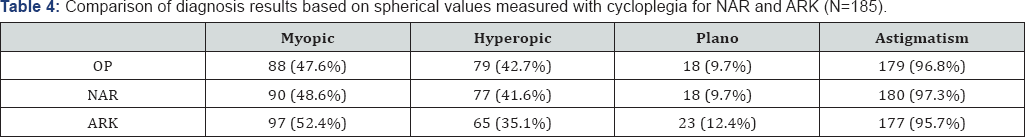
to+10.875). A myopic spherical value was diagnosed in 48.6%, 41.6% were
hyperopic, and 9.7% were Plano. Astigmatism was identified in 97.3%. The
mean spherical value recorded using the ARK on 185eyes was -0.40
diopters, mean cylinder was +0.86 diopters, and mean axis measurement
was 79.95° (Table 2).
The median spherical value was -0.25 diopters (range -6.25 to+10.5).
The mean spherical equivalence measured in this group was +0.05 diopters
(range -4.875 to+10.875). A myopic spherical measurement was diagnosed
in 52.4% of eyes, 35.1% were hyperopic, and 12.4% were Plano.
Astigmatism was identified in 95.7% of eyes (Table 4).
OP: PlusoptiX S04 (Plusoptix GmbH;
Nuremberg, Germany); NAR: Nidek AR-20 (NidekCo.Ltd, Gammagori; Aichi,
Japan); ARK: Nidek ARK-510A (NidekCo.Ltd, Gammagori; Aichi, Japan).
Optix: PlusoptiX S04 (Plusoptix GmbH;
Nuremberg, Germany); C-NAR: cycloplegic-Nidek AR-20 (NidekCo.Ltd,
Gammagori; Aichi, Japan); C-ARK: cycloplegic- Nidek ARK-510A
(NidekCo.Ltd, Gammagori; Aichi, Japan).
Optix: PlusoptiX S04 (Plusoptix GmbH;
Nuremberg, Germany); C-NAR: Cycloplegic- Nidek AR-20 (NidekCo.Ltd,
Gammagori; Aichi, Japan); C-ARK: Cycloplegic- Nidek ARK-510A
(NidekCo.Ltd, Gammagori; Aichi, Japan).
Except, of the axis value, ANOVA testing for auto
refraction parameters of all instruments before cycle plegia revealed no
significant difference among the 3 groups (Table 5).
While paired-samples t-test comparisons of OP and NAR sphere values
showed no statistical significance (p=0.34). Comparisons of sphere
values for OPversus ARK and NAR versus ARKwere statistically significant
(p=0.008 and 0.03 respectively) (Table 5)
. Paired-samples t-test comparisons of cylinder values of NAR versus
ARK showed similar results. However, the OP versus NAR and OP versus ARK
groups showed a significant difference (p= 0.002 and p=0.025
respectively) (Table 5).
The axis value analysis by ANOVA revealed a significant p-value (p=
0.034), indicating an overall significant difference between the 3
groups. Conversely, paired-samples t-test results were only significant
between the NAR and ARK groups (p=0.001) (Table 5).
Calculated spherical equivalence measurements did
correlate with our initial sphere measurements in the NAR versus ARK
groups. Paired-samples t-test comparisons between the OP versus ARK
demonstrated a difference with a p= 0.002. When comparing the OP versus
NAR and the NAR versus ARK groups, no statistical difference was
observed (Table 5).
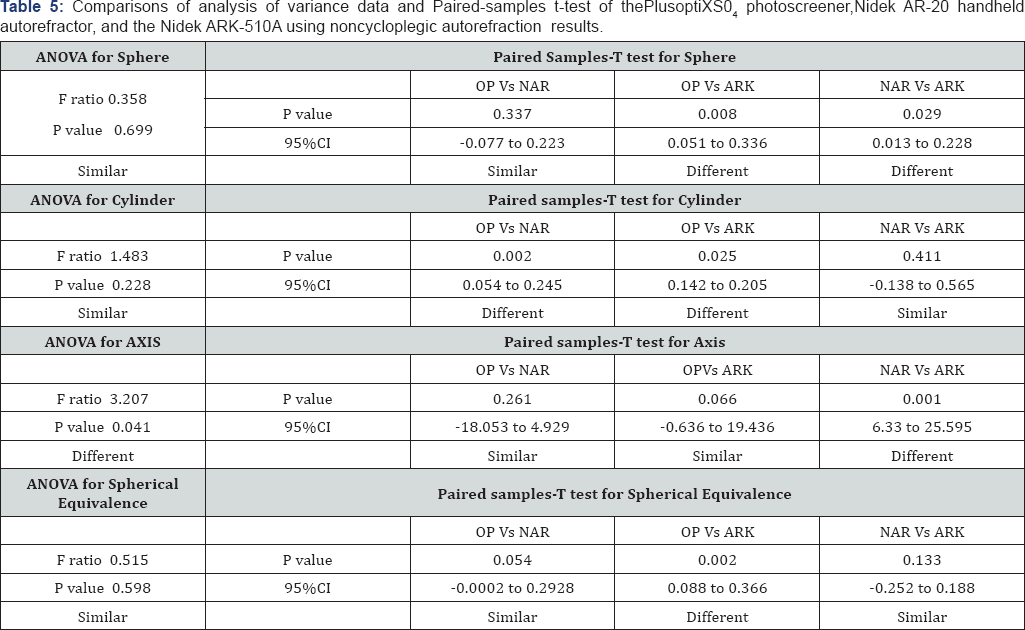
ANOVA: analysis of variance test; CI: confidence
interval; F: Variance ratio; OP: PlusoptiX S04 (Plusoptix GmbH;
Nuremberg, Germany); NAR: Nidek AR-20 (NidekCo.Ltd, Gammagori; Aichi,
Japan); ARK: Nidek ARK-510A (NidekCo.Ltd, Gammagori; Aichi, Japan).
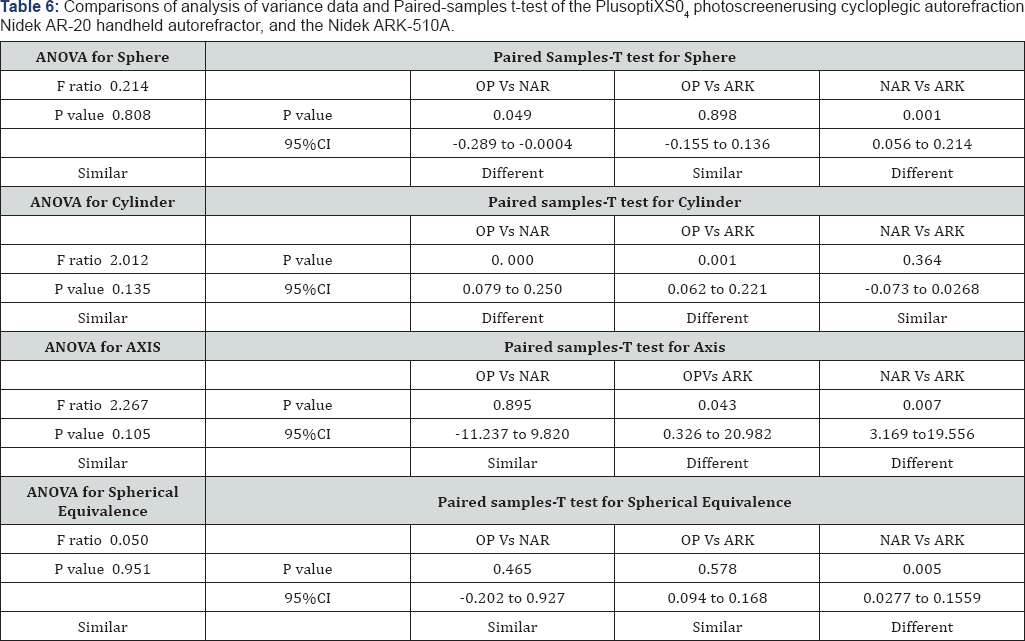
Data from the NAR and ARK instruments were reassessed
using Cyclo pelagic autorefractions (C-NAR and C-ARK); ANOVA testing
for all refraction parameters did not indicate any statistical
differences (Table 6).
Similarly, paired-samples t-test comparisons showed comparable results
among the OP versus C-ARK groups. However, there was a statistical
significance in OP versus C-NAR and C-NAR versus C-ARK groups (p= 0.049
and 0.001 respectively) (Table 6).
Paired-samples t-test for the cylinder values of the OP versus the C -
NAR group and OP versus C-ARK indicated statistical differences (p=0.
000 and p =0. 001) (Table 6).
For Axis values, paired-samples t-test comparisons of
OPversus C-NAR values were statistically similar, whereas those of OP
versus C-ARK showed a significant difference (p= 0.04). The C-NAR axis
value compared to that of the C-ARK also showed a significant difference
(p= 0.07) (Table 6).
Finally, when analyzing spherical equivalence, paired-samples t-test
comparisons showed similar results except for the C-NAR versus C-ARK
group which showed a significant difference with a p=0. 005 (Table 6).
Discussion
Although considered as the gold standard for
measuring refractive status, Cyclo pelagic refractions can be time
consuming, cause patients discomfort and adds additional costs. As
amblyopia is one of the leading causes of visual impairments in adults [13]
developing accurate, easy to use, friendly autorefractors that do not
require the use of cytoplegic agents could help in identifying
significant refractive errors more rapidly and efficiently while
avoiding the drawbacks of cycloplegia.As new instruments for refractive
error measurements become available, it is of critical importance to
evaluate and compare their validity to that of existing reliable
technology. The OP photo screener has been marketed toward health care
providers as a tool to assess refractive errors in young children
without cycloplegia [5,9,10].
Although many studies showed that the OP vision screener is useful as a
screening tool for amblyopia or amblyogenic risk factors [6-10]
Dahlmann-Noor et al argue that the use of OP as a single screening test
in children may miss a significant number of children with amblyopia or
amblyogenic risk factor [14].
As in other studies, we found that both the OP vision
screener and NAR handheld auto refractor were simple and user friendly,
as well as quick in reporting refraction result without the need for
direct contact or patient compliance. However, limitations that we
encountered while using the OP included the need for a dimly lit room to
obtain proper measurements, and its inability to obtain measurements in
patients with a number of ophthalmologic conditions. Of the 19 eyes
that failed autorefraction by the OP, 6 had a high refractive errors
(more than -5), 4 had a history of cataract surgery, 2 had a history of
cataract surgery and corneal rings for keratoconus (also failed
autorefraction by NAR), 2 had a history of diabetic retinopathy, 1 had a
history of a corneal ring for keratoconus, while the remaining 4 had no
known ocular problems but were read as "pupil undetected".
Disadvantages similar to those claimed by Rajavi et al which may have
limited our use included: pupil size, fixation problems and posterior
segment pathologies [15].
Limitations with the NAR were mostly a failure of patient cooperation
resulting in no measurements being taken especially in children. A
child's ability to hold the head still limited our ability to produce
repeatable measurements.
The ARK table-mounted auto refractor readings were more frequently myopic compared to the OP and NAR (Table 3 & 4).
This may be explained by the fact that it is well known that auto
refractive instruments tend to overestimate myopia and underestimate
hyperopia [10].
Except for the axis value prior to cycloplegia, when comparing all 3
instruments using ANOVA, our data indicated that there was no
significant difference in auto refraction results before and after
cyloplegia (Table 5 & 6).
Comparing the OP spherical values with values obtained before
cycloplegia using the NAR and the ARK indicated that there was a
significant difference between the OP and the ARK groups as well as the
NAR and ARK groups. This may lead us to conclude that the two handheld
instruments may not be as reliable as the well established ARK for
diagnosing refractive errors. In contrast, however, the results from
both handheld instruments were similar (Table 5).
Although the above mentioned results were reflected in the calculated
spherical values for both the OP versus ARK and OP versus NAR groups,
the NAR versus the ARK group showed similar results.
After cycloplegia on NAR and ARK, our spherical
values indicated a difference between OP versus C-NAR and the C-NAR
versus C-ARK groups (Tables 6).
However, there was no difference between the OP and C-ARK values. Our
study results are consistent with data from other studies that claim the
OP to be a screening tool to assess refractive without the need
cycloplegia [5,9,10].
While in both the cyclopleged and non cyclopleged groups, the OP
recorded myopia less often than those recorded by the NAR and the ARK,
astigmatism recordings were more comparable in all 3 groups (Table 3 & 4).
The astigmatic (cylinder) readings were statistically similar between
all 3 instruments by ANOVA however, paired samples-T test detected a
difference between the OP and both the NAR and ARK groups before and
after cycloplegia (Table 5 & 6).
These results could mean that with regards to diagnosing astigmatism
(measuring cylinder values) the OP may not be as reliable as the ARK as
compared to the NAR.
Although handheld refractors are proving to be more
practical, time efficient and provide a value as screening tools, we
suggest that they should be used with caution when determining automated
refractions especially in children. In the era of refractive surgery,
it is important to assess the reliability and reproducibility of newer
instruments when compared to existing technology and should not
compromise the accuracy of the refractive state of a patient at the
expense of practicality and time saving. We do not recommend the use of
the hand held instruments for diagnostic purposes, with the exception of
remote or inaccessible areas where portable instruments are essential
and cycloplegia is difficult.
A positive aspect of our study setup is that our
study population was non bias to age during recruitment. To our
knowledge the Optixphotoscreener has only been extensively studied in
screening younger population groups. This study may give us a better
analysis of the use of the open adult patients. Several limitations are
inherent in our study. In view of the time constraints and the
difficulty of getting young children and elderly patients to cooperate
and concentrate for long durations, repeated measurements on all 3
instruments were not documented. Furthermore, and for the same reason of
time constraint, two separate individuals obtaining measurements on the
handheld instruments may have introduced inter-observer bias. Finally,
the same observer documenting measurements from both the handheld and
table-mounted auto refractor was not masked to subjective refraction
readings, introducing possible observer bias.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment