Juniper
Publishers- JOJ Ophthalmology
Introduction
Diseases affecting the cornea are a major cause of blindness all over the world, second only to cataract in overall importance [1].
One of the commonest corneal causes is Infectious Keratitis. The
prevalence of blindness directly resulting from complications of
Infective Keratitis is estimated to be 5% [2].
Cases refractory to the medical therapy requires urgent surgical
intervention to retrieve the vision and most importantly to salvage eye.
Available surgical management in refractory keratitis cases include
tissue adhesives, Bandage Contact Lenses (BCL), penetrating or lamellar
keratoplasty [3]
patch grafts, or conjunctival flaps. Unfortunately, these therapies are
associated with a considerable number of complications and address only
the tectonic problem, without solving the ongoing infection and
inflammation. BCL and conjunctival flaps being a temporary measure does
not provide with new collagen to improve corneal thickness and stabilize
the cornea. For such situations Penetrating Keratoplasty (PK), Lamellar
Keratoplasty (LK) or patch grafts was the only option and is still
being used widely. PK and patch grafts performed to seal a corneal
perforation may be complicated with synechiae, glaucoma, uveitis, and
graft failure in the setting of an inflamed or infected eye [4].
Recurrence of infection in corneal grafts is also challenged. LK being
difficult to perform may result in a double chamber between the donor
and recipient cornea in some cases. Tissue adhesives may dislodge and
are used as a temporary measure, obviating the need for a PK within a
few days [5,6].
Preserved human amnion has been successfully used as
a biological bandage, promoter of epithelialization, inhibitor of
inflammation and angiogenesis, as well as a carrier for ex vivo cultured
limbal stem cells [7].
Amniotic Membrane Transplant (AMT) offers the advantage of avoiding
potential allograft rejection. Even if corneal transplantation is
needed, the success rate is improved if performed on an eye that
underwent AMT reducing inflammation [8,9].
Amniotic Membrane (AM) integrates in cornea and thus can be used as a
treatment for corneal perforation by restoring corneal stromal thickness
so that emergency PK can be avoided, as suitable donor corneal button
availability is difficult in every place. Therefore, an alternative
management for various stages of infectious keratitis including deep
refractory stromal ulcers, descematocele and corneal perforations is
reconstruction of the surface with AMT adjuvant with appropriate
antimicrobials and supportive medications. In this prospective study AMT
in various gravities refractory infective keratitis has been attempted
to understand the efficiencies and limitations associated with it.
Methods
A prospective, interventional study was done on 150
eyes of 150 patients. All patients with refractory (unresponsive to
conventional treatments significantly for more than 2 weeks) infective
keratitis, advanced infectious keratitis with descematocele and corneal
perforation requiring urgent concealment to salvage the eye, were
treated with single or multi layered AMT. Patients with non-infective
ulcers and perforations were excluded from the study. Corneal ulcer was
graded 1-5 according to the depth of corneal involvement on slit lamp
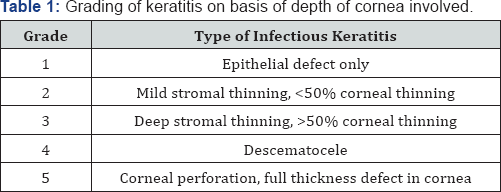
biomicroscopy (Table 1).
Microbial investigations (staining for bacteria and fungus with
culture-sensitivity) were done and antimicrobials started accordingly.
B-scan ultra sonography was done in hazy media to rule out involvement
of posterior segment. Any systemic (diabetes) or ocular (dacryocystitis)
conditions hindering the healing of ulcer or triggering the infection
were investigated and managed.
On basis of slit lamp examination at the site of most impact.
Technique
Surgery was performed preferably under sub
conjunctival or peribulbar anesthesia. In children or uncooperative
patients general anesthesia was used. Debridement of the necrotic tissue
was done from and around the ulcer bed. Care was taken to remove the
pseudo cornea over the perforation at the end of debridement to prevent
leaking of aqueous and thus allowing proper keratectomy. Single layer
preserved AM was used in cases of deep stromal ulcer. AM with epithelial
side up was spread over the ulcer and trimmed to fit the ulcer. It was
secured with continuous or interrupted 10-0 monofilament nylon suture.
Descematocele and small corneal perforations up to 4mm were treated with
multilayer AMT owing to deep corneal involvement. A sheet of AM, folded
over it-self with epithelial side out, filled the ulcer crater and
anchored to the healthy ulcer margin with interrupted 10-0 nylon suture.
It was covered with a single sheet of AM similarly as in cases of deep
stromal ulcers. In large corneal perforations of 4-6mm with extensive
surrounding stromal necrosis, margins were not sturdy to hold the suture
and there was a risk of cutting-off a corneal bite. In such cases
single layer was sutured at limbus to at least provide tectonic support
to the eyeball and delaying the need for PK. Side port or paracentasis
was made in cases hypopyon and corneal perforation to reform the
anterior chamber with air and reposit the prolapsed iris with help of
spatula. Anterior synechiae if present were broken to prevent formation
of adherent leucoma and thereby secondary glaucoma. Hypopyon if present
was washed through the side port and intracameral antibiotic or
antifungal was also injected according to sensitivity. At the end a BCL
was placed over the cornea to prevent irritation from corneal sutures
and maintaining AM in place. Antimicrobial, cycloplegics, ocular
hypotensive and lubricating drops were continued along with systemic
supportive therapy. Frequent follow-ups were done weekly for 1 month,
biweekly till 3 months and monthly till 6 months. Efficacy was monitored
on basis of improvement in symptoms and visual acuity, healing of the
ulcer by re-epithelization and formation of anterior chamber,
achievement of corneal transparency and corneal thickness. Accordingly
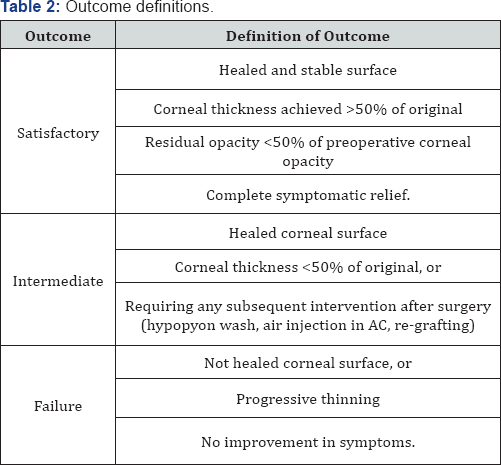
patient's outcome was described as satisfactory, intermediate and
failure (Table 2).
Observation and Results
Keratitis was classified (Table 1)
according to the depth of the cornea involved into 5 grades. Grades 1
and 2 responded well with medical management, therefore did not require
AMT. Grades 3-5 with deeper corneal penetration of infection did not
heal merely with medical management, there was an apprehension of
corneal thinning and progression of infection, which required AMT. Of
the 150 patients who underwent AMT, 55 (36.67%) were deep stromal
ulcers, 25 (16.66%) were descematocele and maximum 70 (46.67%) patients
were of corneal perforation ranging from 1-6mm. There was no age group
or gender preponderance. Symptoms of redness, pain, watering and foreign
body sensation (FBS) were collectively present in all the cases. Lid
oedema and photophobia were also present in majority of the cases (70.6%
and 90% respectively).Presence of discharge was seen in moderately less
cases (30%). ranging between 1-2mm and 10 cases (20%) had hypopyon of
Hypopyon was present in total 50 (33.3 %) cases where 10 cases >2mm (Table 3).
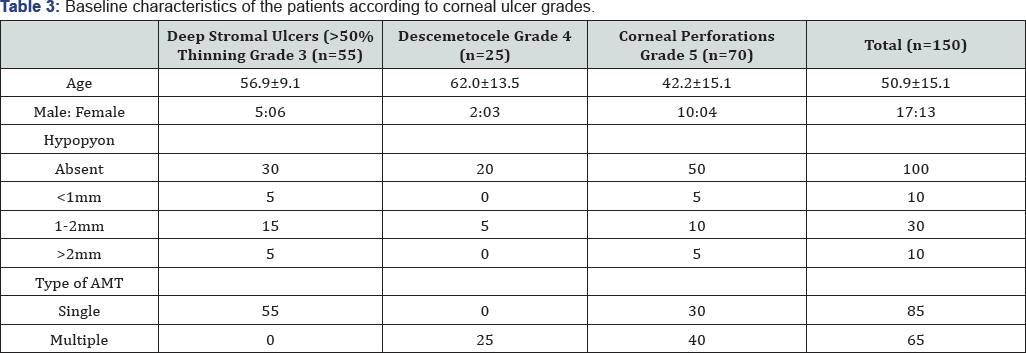
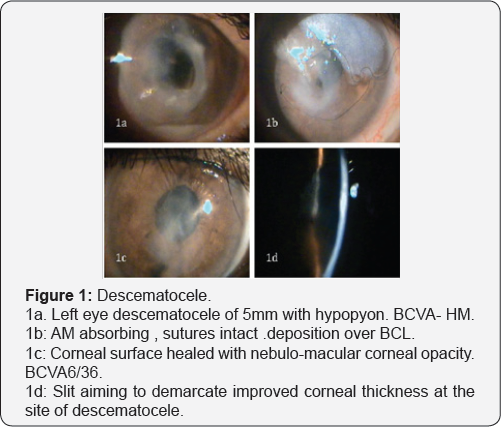
Single layer AMT was done in total 85 cases, all 55
cases of deep stromal ulcer and 30 cases of corneal perforation >4mm
with extensive necrosis to provide tectonic support to maintain
integrity to eyeball. Roofing with multilayer technique was done in 65
cases, all 25 cases of descematocele and 40 cases of corneal perforation
>4mm in largest dimension where neighboring corneal tissue was
healthy to hold the corneal sutures (Table 3). Patients were observed in
repeated postoperative days. Rapid descent of symptoms was observed
after the AMT. There was drastic improvement in pain, lid oedema, FBS
and discharge in the first week. Symptoms were barely present in few
cases by 1 month, which totally recovered by 3 months in all the cases (Figure 1).
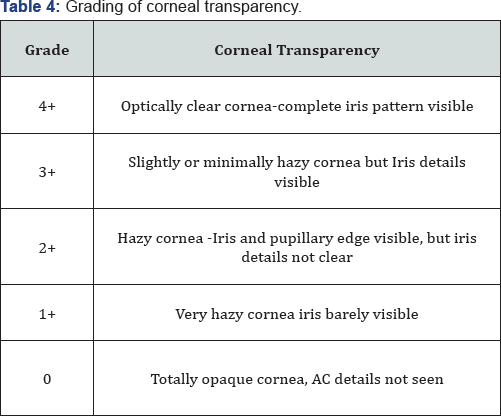
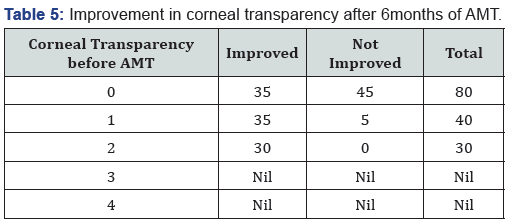
Corneal transparency graded from 0 (leucomatous
opacity) to +4 (clear cornea, with no haze) was measured objectively at
the site of most impact on slit lamp (Table 4).
Improvement was seen in 105 of 150 cases and was statistically
significant (p=0.016). However none of the cases improved to +4
transparency that is totally clear cornea (Table 5).
Visual acuity was recorded before and after 6 months of treatment in
145 of 150 cases as 5 cases of fungal ulcer failed to heal with AMT (Table 6).
Improvement in BCVA when taken collaborate, was extremely significant
(p >0.0001). Mild to moderate complications were faced during the
entire course of treatment. They were shallow anterior chamber in 5
cases in perforation which was tackled with air injection in anterior
chamber and breaking anterior synechiae. Hemorrhage beneath AM in five
cases which resolved spontaneously. Graft retraction was seen in five
cases for which repeat AMT was done. Hypopyon developed in 10 cases and
did not resolve with topical therapy was managed with anterior chamber
wash and intracameral moxifloxacin and amphotericin-B respectively (Table 7).
Hypopyon did not redevelop in these cases. All the complications were
successfully managed with appropriate treatment with no recurrence and
good results. Also no re-infection was noted. Graft melting and corneal
perforation was seen in 5 cases of fulminant fungal ulcer and required
urgent therapeutic PK.


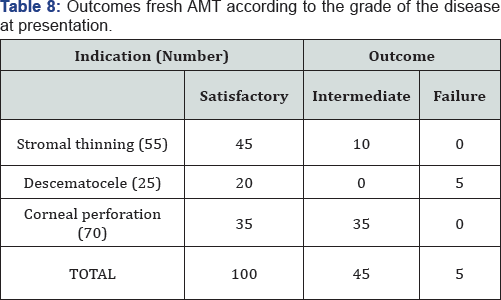
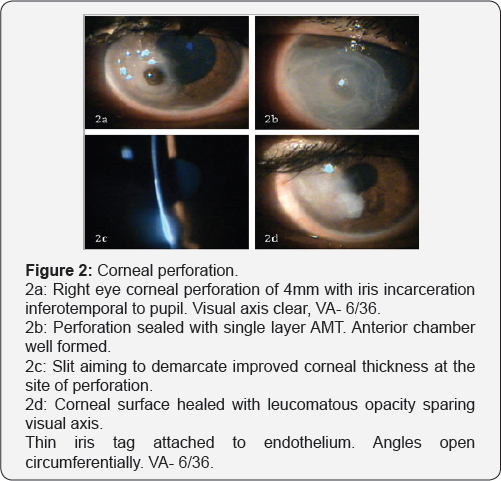
Satisfactory results were seen in 100 of 150 eyes
(66.67%), intermediate results seen in 45 cases (23.33%). Failure was
noted in 5 cases (3.33%) of fulminant fungal ulcers that showed
subsequent corneal perforation requiring Therapeutic PK (Table 8). All
the cases in intermediate category which also required subsequent
intervention, healed with stable cornea. Thus, successful results were
seen in 145 of 150 cases (96.67%) of which in 30 cases subsequent
penetrating keratoplasty was done for leucomatous corneal opacity
obscuring the visual axis left after healed ulcer (Figure 2).
Discussion
Approximately one-third of cases of infective
keratitis require surgical interventions at the acute stage to prevent
perforation or spreading of infection [10-14].
Keratoplasty being majorly followed in such situation faces a
limitation of availability of good quality donor corneas, mainly in
developing countries, recurrence of infection, difficulty in technique
and graft rejection. Moreover, for fungal keratitis PK is technique
dependent and may also carry a risk of recurrent infection [15].
Thus AMT is sought as an alternative, which has been extensively reported in ophthalmology literature [16-19].
AMT offers the advantage of stimulating re-epithelization, preventing
neovascularization and scar formation and avoiding potential allograft
rejection. Even if corneal transplantation is needed, the success rate
is improved if performed on an eye with reduce infection and
inflammation, this can be achieved with AMT [8,9].
In present study complete epithelization was noted in 145 of 150 cases,
that is 96.67% success rate. Similar to our study, Chen et al. [20],
showed 82.61% success rate, 4 of 23 cases in there study faced AM
melting and graft failure requiring therapeutic PK in 3 and delayed
healing with vascularization in the other. Kim et al. [21]
used multilayer AM in cases of descematocele and corneal perforation.
Corneal surface was healed successfully in all cases, and no recurrence
of infection or rejection was experienced. Hanada et al. [22]
used multiple layers of AM for deeper stromal ulcers down to
descemetocele, to restore the normal corneal thickness as well as in
corneal perforations from 0.5 to 3mm with or without additional tissue
adhesive with high success rates (73-93%). In present study corneal
perforations in cases of infectious keratitis up to 6mm have been
treated successfully with AMT alone, and 100% corneal epithelization
with more than 50% corneal thickness have been achieved in all 70 cases
of perforation. In a series by Heiligenhaus et al. [23].
Seven patients with herpes simplex virus or varicella zoster- induced
severe ulcerative keratitis, 5 of 7 eyes healed after first AMT [23]. In another study, stromal defect was filled up with multilayer technique proved to be better than monolayer procedure [22,24,25].
In present study 70% showed significant improvement
in corneal transparency and increasing corneal transparency improves the
best-corrected visual acuity further emphasizing the healing properties
of AMT. Chen et al. [20], preserved useful vision after AMT in cases of fungal keratitis in 52.2% eyes. Kim et al. [21],
reported 21 cases of successful AMT in infectious keratitis, in which
visual acuity increased except for 5 cases because of irreversible
corneal opacity. AMT has come up as a very effective managing technique
for refractory ulcers. It aids in permanent healing of the refractory
infective keratitis and prepares the cornea for definitive
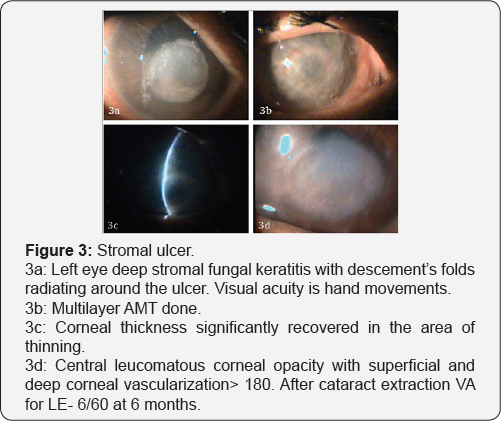
reconstructive procedure if required (Figure 3).
Conclusion
We have found that AMT represents a viable method of
treatment to promote healing and prevent progressive melting of
refractory infectious keratitis. Besides being cost-effective it’s easy
to perform, with a short learning curve. Thus, it might be considered a
first-line surgical technique when maximal medical treatment has failed.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment