Juniper
Publishers- JOJ Ophthalmology
Case Report
A 65-year-old man was referred to the Orbital clinic
from the department of Oral Health, following loss of the orbital floor
and significant parts of the medial and lateral walls, as a result of
maxillectomy for squamous cell carcinoma of the right middle turbinate.
There was no ocular or medical history of note. On examination, his
visual acuities (VA) were 6/9 right eye and 6/5 left eye. He had a right
hypoglobus of 10mm without a palate implant, and 6mm when in-situ.
There was a secondary pseudoupper lid retraction. He had a relative
enophthalmos of 8mm with the implant in-situ. Ocular movements were
full. A HESS chart was recorded (with implant) indicating a right
hypoglobus; diplopia was recorded with red/green glasses, suggesting
image suppression.
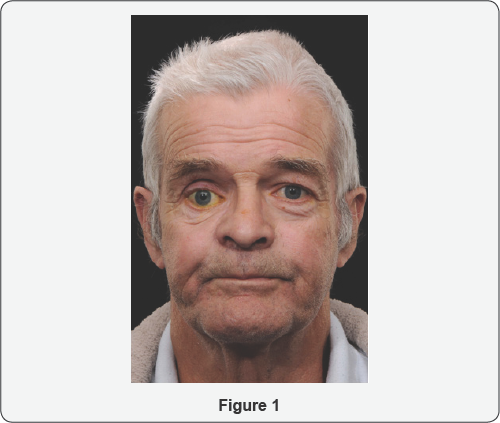
An assessment of his CT scan showed an extensive
hemi- maxillectomy with resection of the orbital floor, much of the
lamin papyracea, the maxillary antrum and hard palate. Significant
enophthalmos was noted. Soft tissue thickening in the region of the
surgical margins was noted (Figure 1).
As the patient had undergone post-operative radiotherapy, a
conservative approach using NASHA for volume augmentation was decided as
an initial step. Floor and medial wall reconstruction with
implant/dermo fat graft at the level of the equator of orbit was
deferred following discussion with the patient. Correction of lid
position would be deferred until later.
He underwent an injection of Orbital (non-animal
stabilized hyaluronic acid) NASHA. Retrobulbar block was used comprising
of Lignocaine 2% with adrenaline 1:200000; 1.5mls was injected, deep,
below the globe. The plunger was initially withdrawn to ensure blood
vessels were not entered, and a staged augmentation was performed, Three
mls of Perlane (Q-Med, Uppsala, Sweden) was injected above the
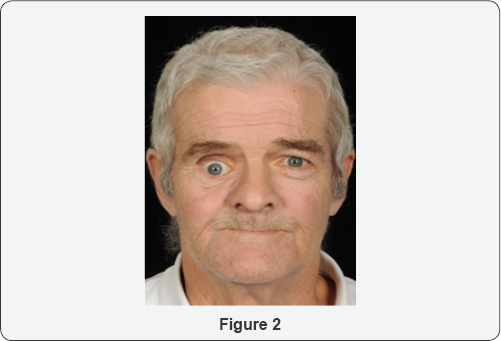
periorbitum of the floor, using an 18G needle. Immediately after the
procedure, vision and optic nerve function were monitored and were
normal (Compare Figures 2 &3).

At review 1-week later, a 3mm improvement in
hyppoglobus and 4mm improvement in enophthalmos was noted. However, he
was aware of vertical diplopia, and this was controlled with a base-
down 3-dioptre prism. This was thought to be due to loss of right eye
suppression with the new globe position.
A further review was performed at 8-months
post-injection and a slight increase in enophthalmos and hypoglobus were
noted.At 13-months after the initial injection, encouraged by initial
results, a further injection of 3mls of Perlane (Q-Med, Uppsala, Sweden)
was injected using the same technique as before with tightening of the
lower lid by means of a lateral canthal elevation. This resulted in an
improvement in hypoglobus to 2-3mm. His diplopia persisted without
prisms, although over the next 8-months started coping better without
prisms and the diplopia resolved with normal binocular single vision.
The long-term plan was to continue with annual orbital NASHA injections
Discussion
From an ophthalmic point of view, mid-face
reconstruction aims to provide support to orbital contents, minimize
changes in globe position, orbital volume and eyelid function [1].
Symmetrical orbital volume is a requirement for binocular single
vision. Complications following reconstructive surgery, and
radiotherapy, include resorption of orbital fat and wound contracture,
exacerbating enophthalmos and diplopia. Post-maxillectomy radiation
therapy increases the risk of orbital sequelae, such as fat atrophy and
scar formation, and ocular sequelae, such as optic atrophy, cataract
formation, ocular surface dryness, and ectropion [2].
Orbital reconstruction may range from minimal to
complex. Minimal bone resections or small orbital floor defects may not
require reconstruction. On the other end of the spectrum, subtotal/
total floor defects (>75% surface area) and multi segmental defects
will necessitate rigid reconstruction. Primary reconstruction of total
maxillectomy defects with preservation of orbital contents remains a
complex problem without a perfect solution [3]. In a case series of 66 patients with sinonasal malignancy that had eye-sparing surgery, [2]
the most common abnormality following subsequent reconstruction was
globe mal position (enophthalmos or hypophthalmos) (34/66 patients,
63%), associated with lack of adequate rigid reconstruction of subtotal
or total orbital floor or multisegment orbital defects [2]. The problem can be exacerbated with post-operative radiotherapy [4].
In our case, the patient was keen for correction of
his vertical dystopia from a functional and cosmetic point of view.
Surgery would have been quite complex due to the absence of the floor,
medial and lateral walls. The option of volume augmenatation with a
dermo fat graft was considered, but there was a possibility that this
graft might not survive due to lack of circulation. There was also a
risk of recurrence of the original pathology. A conservative approach
was taken and floor augmentation with NASHA was decided as the first
stage of the procedure. This addressed both the hypoglobus and
enophthalmos to the patient's satisfaction, to the extent that need for
further orbital surgery was obviated. Furthermore, binocular single
vision returned with the use of prisms.
There are no reports addressing reconstruction of the
orbital component of the post-maxillectomy defect using injectable
materials for volume augmentation that we are aware of. A minimally
invasive approach to orbital volume augmentation using agents such as
injectable calcium hydroxylapatite (CaHA), polyacrylamide gel, hydrogel
pellet expanders, micro-fat grafts and NASHA have been well described in
the anophthalmic socket (post-enucleation socket syndrome). There are
only a handful of reports in the context of sighted globes. These
include silent sinus syndrome, [5] deep set eyes, [6,7] trauma, [7] and facial hemiatrophy (Parry Romberg syndrome) [7]. We are not aware of any reports of use of filler in the context of carcinoma.
NASHA is produced from non-animal sources by
bacterial fermentation. It is well tolerated, has a low immunogenic
potential, and there is low risk ofantigenic contamination and
hypersensitivity reactions [8].
A major advantage in sighted globes is that its effects can be reversed
by dissolving it with hyaluronidase. Disadvantages include a relatively
short life span compared to other products and the requirement to
inject through an 18G needle in order to maintain particle integrity [8].
However, blunt cannulas can be used. Some studies have reported a 1:1
correlation between the desired augmentation volume (enophthalmos
reduction) and each millimetre of product injected, [7] whilst others have not [9].
(We feel the augmentation effect depends on the remaining bony walls
and the integrity of the periorbita). Twelve months is the longest
duration of action reported [7,9].
Injection of NASHA is recommended in the anterior orbit, and behind the
equator of the globe, in order to achieve globe elevation and axial
globe advancement respectively [7,9,10].
Injections may be intraconal or extraconal. Proponents of the former
cite better globe advancement and reduced anterior migration of filler; [11] proponents of the latter cite risk of vascular compression in sighted globes with intraconal placement [8].
Possible complications include risk of intravascular
injection and embolization with loss of vision in sighted eyes. Commonly
reported complications include injection site tenderness, ecchymosis
and chemosis, [12] stimulation of oculocardiac reflex and associated hypotension, [7,8,12] transient ptosis, [6] anterior migration of filler [13] and inflammatory orbital cellulitis [9].
The benefits of a minimally invasive approach over
traditional surgery include reduced operating times, application under
local anaesthesia, reduced recovery time and reduced risk of host and
donor site morbidity where non-biological materials are used. The
benefits need to be weighed against the risks. In the setting of
post-neoplasia reconstruction where the prognosis may be poor, use of
minimally invasive, albeit temporary, techniques can help to the improve
quality and dignity of life for patients, especially where resorting to
more complex surgical procedures may be too demanding for the patient
in view of their morbidity and reduced life-expectancy [14].
In summary, injectable fillers can provide a
temporary solution to volume augmentation of the orbit, for functional
restoration and improvement in cosmesis; and may be used in sighted
globes with caution. They may be a superior option to traditional
surgery in selected cases.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment