Juniper
Publishers- JOJ Ophthalmology
Introduction
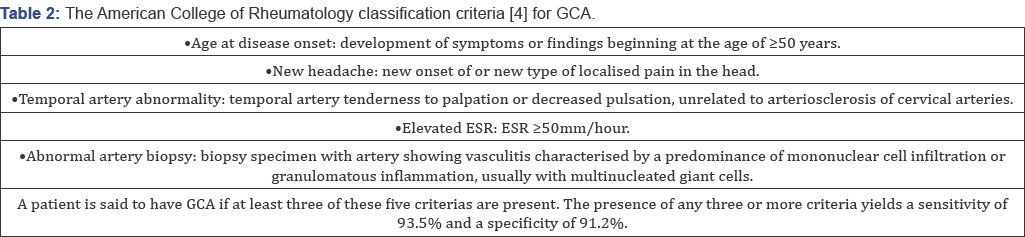
Giant cell arteritis (GCA), is a systemic vasculitis, affects medium and large sized cranial arteries [1], it can cause serious morbidities. Giant cell arteritis (GCA) predominantly affects elderly females [2].
The typical symptoms of new-onset GCA are bitemporal headaches, jaw
claudiacation, scalp tenderness, visual disturbances, systemic symptoms
such as fever and weight loss, and polymyalgia [3].
The diagnostic assessment comprises laboratory testing (erythrocyte
sedimentation rate, C-reactive protein), temporal artery biopsy and
imaging studies. The most important complication is permenant and deep
vision loss. Diagnosis of TA is difficult if typical symptoms other than
visual loss are absent. It can be difficult to diagnose this disease in
the absence of typical clinical signs and labaratuary findings. Here we
report a silent and atypical temporal arteritis case (Table 1& 2).
Case Report
63 year old hypertensive male patient applied to our hospital with complaint of vision loss in his right eye for two
weeks. His visual acquity was perception of hand
movements in right eye and 8/10 according to Snellen Chart in left eye.
While anterior segment evaluation revealed bilateral nuclear sclerosis,
fundoscopic examination revealed papiledema in his right eye. He did not
complain of any associated headache, scalp tenderness, jaw claudication
or constitutional symptoms such as weight loss, fever, malaise or
sweats. We consulted the patient to internal medicine, rheumotology and
hematology departments. His clinical and labaratuary findings were
unremarkable except thrombocytosis. Following a presumptive diagnosis of
non- arteritic ischemic optic neuropathy the patient was hospitalized
and treated with intravenous 1000mg methylprednisolone for 3 days. After
3 days, oral prednisolone therapy was started 60mg per day. Oral
steroid therapy was tapered 10mg with 3 days interval. However at
10-days' examination visual acquity in his right eye was reduced to loss
of light perception. 1 month later, patient presented with sudden
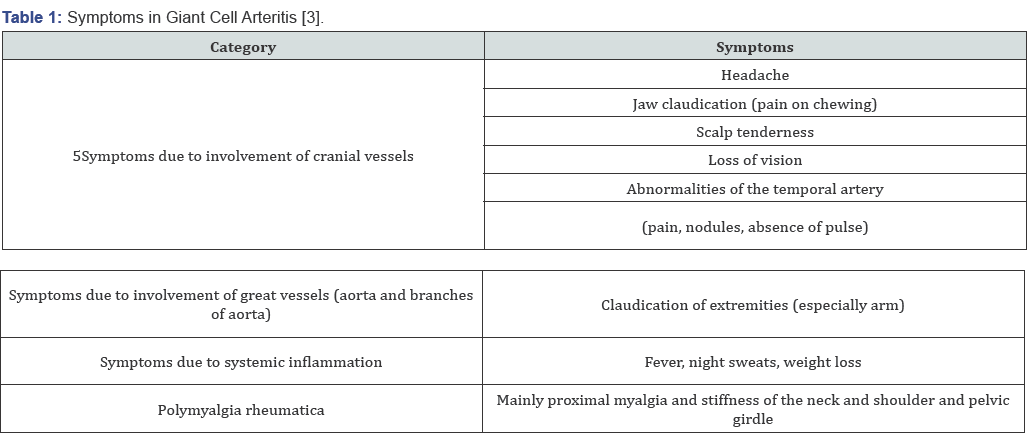
vision loss in his left eye, headache and malaise. Fundus examination
revealed left optic disc swelling and soft exudates near the optic disc (Figure 1).
Floroscein anjiography showed delayed filling at arterial phase and
late staining of the optic disc. When labaratuary tests were repeated,
erythrocyte sedimentation rate (ESR) was 65mm/ h(normal range: 1-15mm/h)
and creactive protein (CRP) level was 15mg/L (normal range: <5
mg/L). According to these findings, with the diagnosis of arteritic
ischemic optic neuropathy, intravenous steroid therapy was initiated.
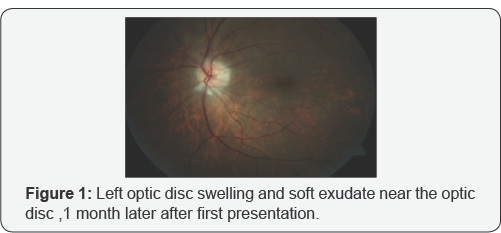
Rheumatology department evaluated the patient again and a temporal
artery biopsy was performed; focal chronic inflammation and elastic
fiber degeneration areas were identified at histologic sections (Figure 2).
At the fifth day of intravenous steroid therapy visual acquity in left
eye was 7/10 according to the Snellen Chart. The Humphrey Perimetry test
revealed a paracentral island in his left eye.Since the visual acquity
was at the level of loss of light perception at the right eye we didn't
perform the Humphrey Perimetry test for the right eye.

Discussion
Patients with GCA typically present headache, jaw
claudication, fever, weight loss, myalgia, arthralgia or malaise.
Conversely, patients with occult GCA, first described by Simmons &
Cogan [5],
present with sudden visual loss without systemic symptoms and signs.
Thus, due to the lack of symptoms, diagnosis and treatment of silent GCA
may be considerably delayed when compared to typical GCA. Occult GCA , a
potential cause of blindness, is defined as ocular involvement of GCA
without any systemic symptoms and signs [6]. Ocular symptoms include visual loss, amaurosis fugax, diplopia and eye pain Hayreh et al. [6], described cotton wool spots in up to one third of eyes with visual loss dring the early stages of occult GCA [6].
Scalp abcess, chronic earache, bilateral central retinal artery
occlusion, mydriaitic pupil, dry cough, aort anevrism , bilateral
submandibular lymphadenopathy, hepatosplenomegaly are some atypic
symptoms of GCA. The occult GCA group had higher C-reactive protein
levels, a higher platelet count , and lower serum albumin levels [7].
Ophthalmic involvement can occur in up to 50% to 70% of the GCA
patients, and this represents an ocular emergency. Arteritic anterior
ischemic optic neuropathy (AAION) is the most common type of ophthalmic
involvement in GCA and can cause permanent visual loss. Therefore,
prompt diagnosis and treatment with a high dose of steroids is essential
for these patients. In our patient at the first presentation
labaratuary findings were unremarkable and there were no systemic
symptoms; therefore at the beginning, our presumptive diagnosis was
non-arteritic ischemic optic neuropathy of right eye. 1 month later,
sudden vision loss appeared at left eye and he was complaining from
headache, scalp tenderness ; ESR and CRP levels were elevated on
labaratuary examination at that time. Hayreh et al. [6]
found that ESR and CRP levels were relatively lower in patients with
occult GCA compared to cranial GCA. On the other hand, Hamidou et al. [7]
found higher CRP levels, a higher platelet count, and lower serum
albumin levels in occult GCA group. In our patient's first presentation,
ESR and CRP levels were within the normal limits. One month later when
the other eye was effected ESR and CRP levels were remarkably high (Figure 3].

Although Liozon et al. [8]
describes occult GCA as a protracted inflammatory response and a
relatively benign short term outcome, in our case despite the long term
corticosteroid and immunsupresive treatment, visual acquity was loss of
light perception level in the right eye. Tan et al. [9]
reported a case of GCA involving only the occipital artery which was
revealed by magnetic resonance angiography. Chomlak et al. [10] reported a case of GCA with vertebral artery involvement, which was refractory to immunosuppressives. Hocevar et al. [11]
claimed that, even early diagnosis and a prompt initiation of steroid
did not prevent relapses in GCA. In our case after first attack despite
the prompt intravenous steroid therapy one month later the patient
consulted with visual loss at his other eye this verified Hocevar’s
hypothesis. Cullen et al. [12] reported an occult GCA case in Singapore. Papakostas et al. [13]
reported a case of GCA that presented with cotton wool spots and
retinal vasculitis affecting small-size retinal arterioles. Shambhu et
al. [14]
reported an atypical case of GCA presenting as mild upper abdominal
pain and generalized weakness in the context of hyponatremia as the
presenting manifestation of vasculitis that was subsequently diagnosed
by MRI scanning. Cheema et al. [15]
described a case had the signs and symptoms consistent with GCA but who
had an ESR within the normal limits, 27mm/h. In our case ESR at the
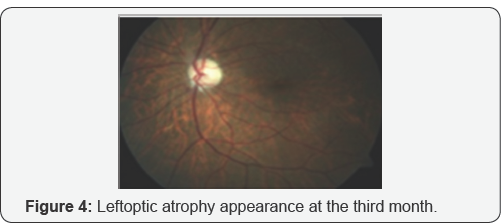
first presenting ESR was within the normal limits,too. Labarca et al. [16] reported that patients with hypertension or diabetes at GCA diagnosis have more relapses during follow-up. Kermani et al. [17] reported seven patients with a positive temporal arteritis for GCA had a normal ESR and CRP at diagnosis (Figure 4].
In people older than 55 years, amaurosis fugax or
visual loss, development of an acute ocular ischemic lesion with or
without elevated erythrocyte sedimentation rate and systemic symptoms,
should raise suspicion for giant cell arteritis. The diagnosis of
temporal arteritis is easily made when sudden loss is contemporary with
other symptoms and raised inflammatory markers. In the absence of known
symptoms, in a patient diagnosed as ischemic optic neuropathy, occult
temporal arteritis shouldn’t be out of mind. Despite the early diagnosis
and treatment final visual acquity may not be satisfactory.
Conflict of Interest
Asfuroglu declares that he has no conflict of
interest. Author Koz declares that she has no conflict of interest.
Author Ozbalkan declares that she has no conflict of interest. Author
Sandikci declares that she has no conflict of interest. Author Ciftci
declares that she has no conflict of interest. Author Ozdemir declares
that she has no conflict of interest.
This article does not contain any studies with human participant performed by any of the authors.
Informed consent was obtained from all individual participants included in the study.
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
No comments:
Post a Comment