Juniper
Publishers- JOJ Ophthalmology
Binocular vision is the fundamental refinement of the
visual function. It has 3 degrees: spontaneous vision, fusion, and
stereoscopic vision. Stereopsis refers to the ability of the visual
function to perceive depths and landscapes using binocular vision [
1]. Stereoscopic acuity measured by the smallest detected retinal disparity [
1], gives clear indication of the quality of binocular vision of an individual [
2].
At adulthood, the absence of binocular vision can have an impact on
professional orientation. People affected are excluded from certain
professions as in aeronautics, marine and military careers: police, fire
fighters. The very young child without binocular vision has at times
difficulty learning how to walk, to read, or even how to write. A
reduction in stereoscopic acuity can be associated to a number of vision
problems as strabismus, amblyopia and anisometropia. As such, the
measurement of stereoscopic acuity is frequently used to screen for
visual dysfunction in children. It is more reliable than visual acuity
in the screening of amblyopia [
3].Stereoscopic
vision continues to evolve after birth. According to a number of
authors, the maturation of stereoscopic vision is almost complete in
children between 3 and 5 years [
4-
6].
In view of the importance of this characteristic, we aimed at
establishing the profile of stereoscopic acuity of schooling children
aged 3 to 5 years in the Yaounde 2 sub-division.
We conducted a cross-sectional descriptive study from
March 13 to May 15, 2015 in 10 nursery schools of the Yaounde 2
subdivision. Were included all schooling children aged 3 to 5 years who
obtained written informed consent from their parents. Were excluded from
our study all non-cooperating children after numerous trials or sick on
the day of the descent, or refusal from parents. To obtain our sample
size, we used probabilistic sampling in 4 degrees. Raffle draw permitted
to choose Yaounde 2 sub-division amongst the seven M foundi divisions.
For the 2nd degree which concerned the choice of the 10
schools amongst the 86 schools of the Yaounde 2 sub-division, we used
Excel 2010. By random draw, a class was chosen per section. As for the 4th
degree, the choice of children in the classes. We agreed on a
systematic draw of the first 20 pair numbers according to the order of
the class list, which followed the order of registration in school. In
total, we chose 600 children. We sent 600 questionnaires with
notification letters and informed consent forms to the parents of the
pupils chosen 3 days before our visit to the school.
This was done in 4 steps. Firstly, hetero-anamnesis
of children from their parents, using the pre-prepared questionnaire
filled at home by themselves. We looked for neonatal and
ophthalmological past medical history. Then was general inspection
performed with emphasis on eyes, looking for malformation, torticollis,
nystagmus, apparent strabismus, or an abnormality of the cornea. After
this we undertook, measurement of distance visual acuity with and
without optic correction using Pigassou's scale placed 5 metres in front
of the child. At the end came evaluation of stereoscopic vision using
Stereo test TNO. The child with duo chromic lenses (red/green), the test
placed at 40cm away from his/her eyes, perpendicular to the visual
axis, the different plates were moved in front of them so that they
should identify. Significant reduction of distance visual acuity (RdVA)
was defined by distance visual acuity, dVA≤6/10 in at least one eye or
an anisoacuity≥2 line on Pigassou's scale stereoscopic acuity, SA≥240”
corresponded to an abnormal or bad stereoscopic vision.
Data collected was entered in a database created with
CSPro 6.0 software and were exported to IBM SPSS 21 software. Tables
and diagrams were designed using Excel 2010. Anova test was used to
compare the stereo acuity between different age groups and Pearson's Chi2test and Fischer Exact test to look for associated factors to bad stereoscopic vision. Significance was set at 0.05.
We sent 600 questionnaires together with informed
consent forms to parents of selected pupils. We registered 374 forms
amongst which 6 refusal and 3 absences. Our analysis was on 365 children
in total; a participation rate of 60.8%.
Among the 365 children examined, 175 were girls
(47.9%) and 190 boys (52.1%), with a sex-ratio of 1.1 in favour of boys.
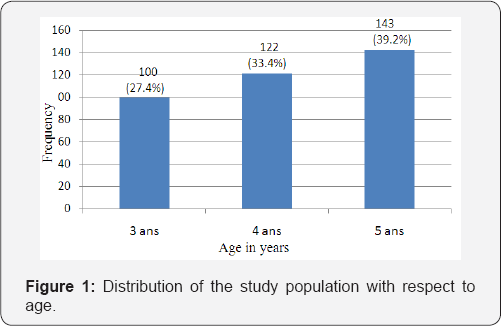
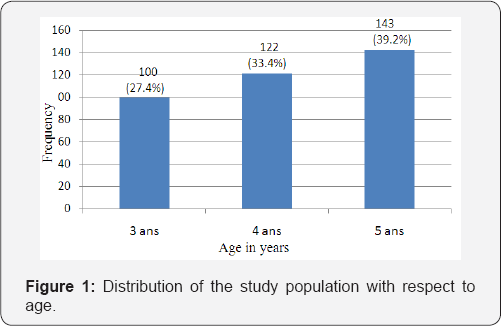
Our population was divided in 03 groups: 100 (27.4%) children aged 3
years, 122 (33.4%) aged 4 years, and 143 (39.2%) aged 5 years (
Figure 1). The most represented age group was that of 5 years. The mean age was 4.2±0.81 years.
In the past-history mostly mentioned were prematurity 11cases, trauma 8 cases, and eye redness 6 cases.
At general examination, 4 children had strabismus, 2
others a vicious position of the head and one presented a nystagmus. We
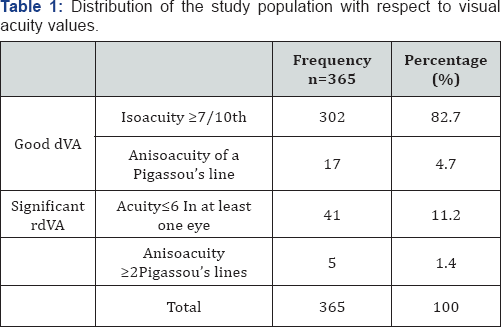
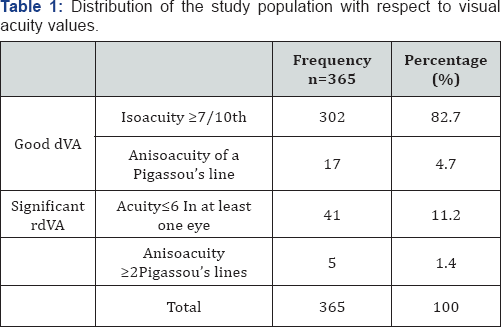
also found 2 children with optic corrections. Distance visual acuity was
normal in 319 children (87.4%), (
Table 1). The children had a poor distance visual acuity, represented 12.6% of the study population.
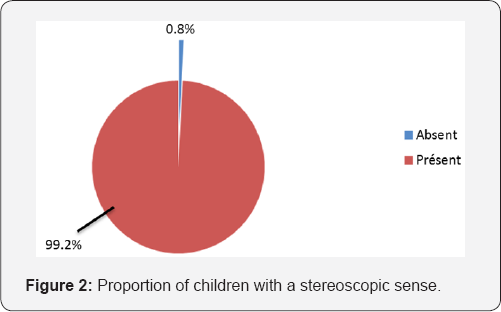
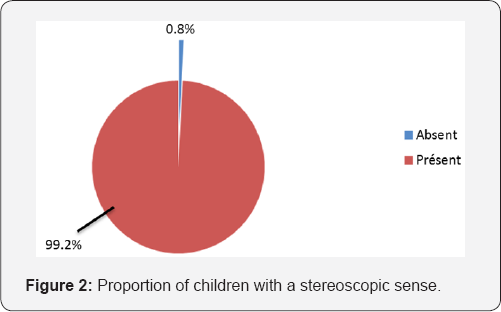
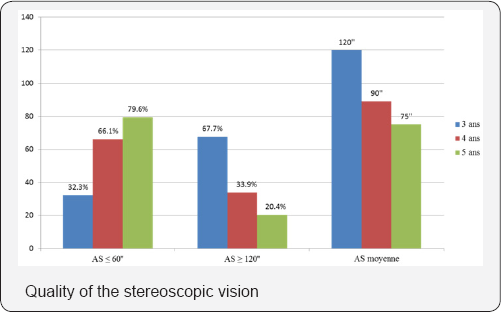
In our study population, 99.2% (362 children) had the stereoscopic sense as represented by (
Figure 2).
In 03 (0.8%) cases, we discovered an absence of stereoscopy; one in
each age- group. Among the 3 children (0.8%), with ocular dominance,2
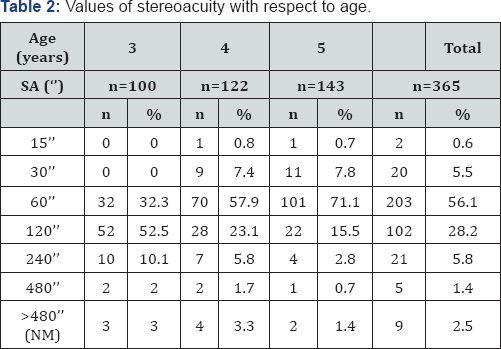
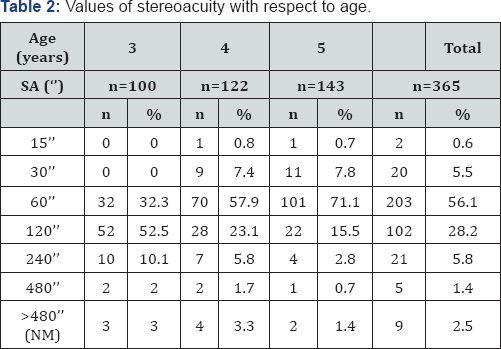
had left eye dominance. The value of stereoacuity (SA) with the largest
proportion was 60"; 56.1% (203) of the study population. We counted 102
children (28.2%) with SA of 120" The least represented class was that of
15", 2 (0.6%) (
Table 2).
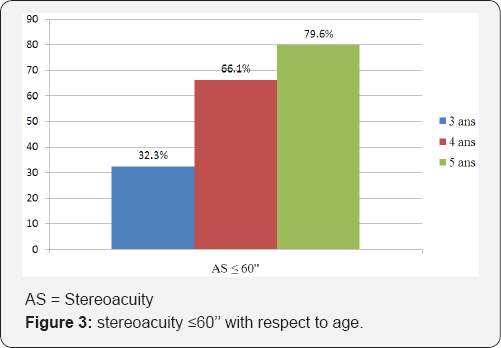
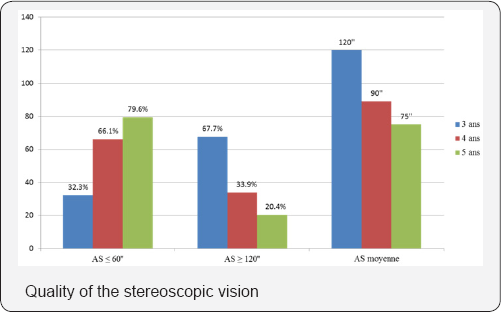
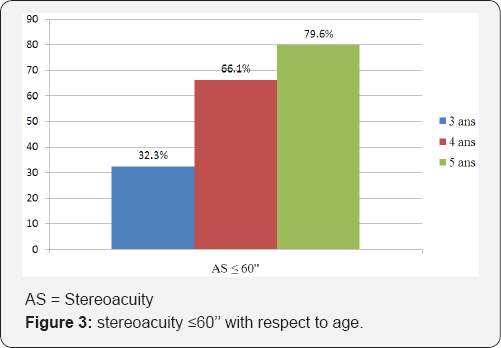
The proportion of children with SA <60" increased with age, 32
children (32.3%) amongst those aged 3 years, 80 (66.1%) in those aged 4
years, and 113 (79.6%) amongst the group of children aged 5 years. This
increase in percentages with age was statistically significant (p=0.000)
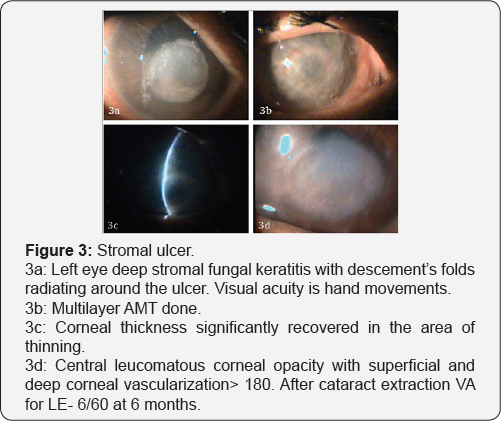
(
Figure 3).
The tendency inverted with values of 120" to 480", the proportions
decreased with age. These differences were statistically significant
with p=0.000. The median values of stereoacuity gradually sharpened with
age. They varied between 120" at 3 year, to 60" at 4 and 5 years. This
variation was statistically significant (p=0.000).
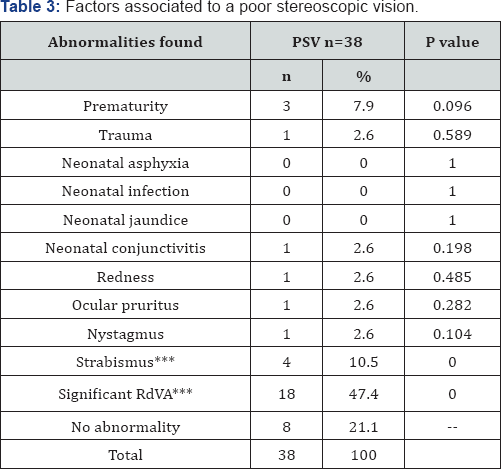
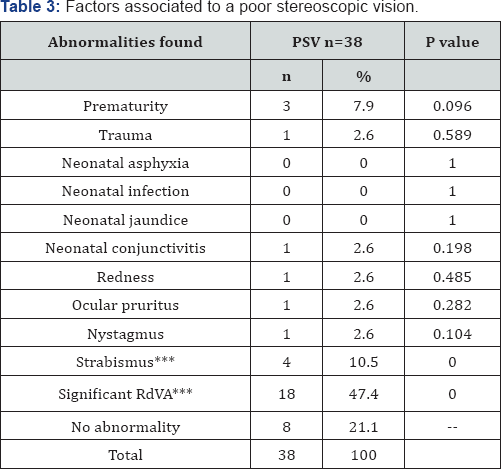
In total, we found poor stereoscopic vision in 38 children, 10.4% of the study population (
Table 2).
According to the fact that age increased, the percentage of children
with a normal stereoscopic vision increased and inversely, the
proportion of children with poor stereoscopic vision decreased,
significantly (p=0.000). The significant Reduction in distance visual
acuity (RdVA) and strabismus were the most encountered abnormalities in
the group of children with poor stereoscopic vision (>240"), with
respective percentages of 47.4% and 10.5% (
Table 3).
After bivariate analysis, these two abnormalities were identified as
being associated to poor stereoscopic vision with a p=0.000 (
Table 3).
The principal objective of this study was to
establish the profile of stereoscopic vision of schooling children aged 3
to 5 years of the Yaounde 2 sub-division. Specifically, it aimed at
determining the proportion of children with the stereoscopic sense, to
measure the median values of stereoacuity and finally, to distinguish
the factors associated to poor stereoscopic vision in our study
population.
A total of 600 forms were distributed and only 365
children were examined, giving a participation rate of 60.8%. This rate
was less than that obtained in the North department of France, during
the 2011-2012 vision campaign organized by APESAL (Association de
Prévention Et de Dépistage de troubles visuels Actions Locales) [
7].
During this campaign in favour of children aged 2 years and a half to 3
years and a half, the participation rate was 80.05%. This difference
could be explained by the fact that the French health system encourages
screening of childhood visual disorders. It could also be due to the
level of alphabetisation of Cameroon (71.3% according to the 3
rd global population census and of habitat of Cameroon) [
8],
which is less than that of France (99%, according to the Institute
national de la statistique et des étudeséconomiques). Moreover,
screening campaigns in France are scheduled well ahead of time and
introduced in the calendar of targeted schools. Parents are informed
many times for their participation. On the other hand, our study took
place on a short period. The delay between distribution of forms and the
field work was just 02 days, and no reminder was sent to parents. Also,
we can add the skepticism of certain parents.
We targeted children aged 3 to 5 years. Given that
the schooling rate of the populations of Yaounde is 88.8% according to
the results of the Demographic and health investigation and having
multiple indicators done in 2011 (EDS 2011) [
9],
the majority of children aged 3 to 5 years of Yaounde are in school at
least 5 hours per day. That is why the site of recruitment chosen was
nursery schools. In nursery schools, we generally find children from 3
years. However, many are those who will celebrate their birthday during
the school year. Thus, in the small section, we can find children of 4
years, same for the midsection with children of 5 years. This could
explain why in our study population, children aged 5 years were more
represented (39.2%), whereas the least represented were those aged 3
years (27.4%), with a mean age of 4.12±0.81 years.
According to our results, 0.8% of children didn't
have the stereoscopic sense. The study Vision in Preschoolers (VIP),
Ciner et al. [
5]
in the USA, on the stereoscopic acuity of children of 3 to 5 years,
reported that 1.0% of children of the age range did not have the
stereoscopic sense [
5],
results with corroborates ours. Moreover, he mentions that the
proportion of children without the stereoscopic sense increased with
age. Our sample respected this finding but this tendency was not
statistically significant (p=0.800), which could be due to our sample
which is smaller than that of Ciner et al.
In our sample, measured with the stereo test TNO, the
cumulative percentages of children with stereo acuity<60" was 32.3%
at 3 years, 66.1% at 4 years and 79.6% at 5 years. This increasing
tendency with age was statistically significant (p=0.000). The TNO
measures disparities till 15". Our results are similar to those of Ciner
et al. [
5]
who using the Stereo Smile II whose finest measured disparity is 60".
He compared the stereo acuity among age groups (3, 4 and 5 years) and
between the group of children with and without any disorder. His study
population was made up of children from the Vision in Pre-schoolers
programme. He reports that the proportions of children having reached
that disparity increased significantly with age. Thus, 52.2% of the 3
years, 64.9% of the 4 years, and 71.4% of the 5 years were able to see
in landscape with an SA ≤60" [
5].The
median SA of schooling children aged 3 to 5 years in Yaounde 2 varied
from 120" to 60", respectively from 3 years, to 4 and 5 years. This
improvement with age was statistically significant (p=0.000). In 1975,
Romano conducted his study using Titmus stereotest. He found median
disparities from 200", 90" and 40" respectively for 3 years, 4 years and
5 years [
6]. Likewise, Birch et al. [
10]
in 2008, using the Randot stereo acuity test observed that the median
values of SA sharpened with age, going from 100" at 3 years, to 60" at 5
years [
10].
Thus, the median of SA with respect to age that we calculated sharpened
with age, as described by the previous authors irrespective of the test
used. Thus, the thresholds of SA for children of 3 to 5 years are very
close to those found in adults suggesting therefore the maturation of
stereoscopic vision is almost complete in children of that age range.
The number of children per age group, with poor
stereoscopic vision, progressively significantly decreased with age
increase. Fifteen percent of the population aged 3 years presented with a
poor stereoscopic vision, 10.7% of 4 years, and 4.9% of 5 years
(p=0.000). Ciner suggested the same variation in 2014: 29.6% at 3 years,
22.5% at 4 years, and 19.2% at 5 years [
5].
The greatest proportions registered by his group could be due to the
fact that his study population was far greater than ours, and had a
large number of children suffering from at least one vision disorder
which could hamper stereopsis.
We detected 4 cases of strabismus. All of them had a
poor stereoscopic vision, representing 10.5% of children with abnormal
stereoscopic vision. An association was established between strabismus
and abnormal stereoscopic vision (p=0.000). This corroborates what many
authors have described [
5,
11].
Sharma et al conducted a case-control study. They compared the SA of
strabismus patients to that of a control. They showed a significant
(p<0.001) poor stereopsis in the strabismus patients [
11].The
presence of a reduction in distance visual acuity (RdVA) was an
associated factor to poor stereoscopic vision (p=0.000). This
association is in the same line with reports from Ciner in 2014. Indeed,
he found values of SA≥240" in 40.7% of children with a reduction in
distance visual acuity (p<0.05) [
5].
Amongst the children with poor stereo acuity, we identified 3 premature
births (7.9%). According to our findings, prematurity does not
influence stereoscopic vision (p>0.05). In 2000, Hard et al. [
12]
worked on a population of 51 premature children with mean age of
7.2±2.1 years. He showed that this population had an important
prevalence of vision disorders, such as altered stereoscopic vision,
associated or not to strabismus. Hard counted 7 children with a
pathological stereoacuity, among the 31-extreme premature (GA<28
weeks), giving a prevalence of 22.6% [
11].
This disagreement between the two studies could be explained by our
sample size. It is small and the risk groups, notably the premature
children, were not sufficiently represented.
The profile of stereoacuity in Cameroonian children
does not present any specificity with respect to literature.
Stereoacuity continues to sharpen between 3 and 5 years to reach adult
threshold values. This test is recommended for the screening of
childhood vision disorders for it is more reliable than the measurement
of visual acuity in the screening of morbidities such as strabismus and
amblyopia.